Abstract
Introduction
Patterns of worldwide immigration have resulted in high rates of discordance between medical providers and the patients they treat. For example, in the USA, 25 million individuals in the USA self-identified that they speak English less than “very well.” Previous studies have generated mixed results regarding differences in postoperative outcomes between English proficient (EP) and limited English proficient (LEP) patients. Our objective was to determine whether a difference in outcomes exists for non-English-speaking patients compared to English-speaking patients after operations commonly performed to treat cancer.
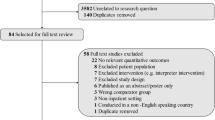
Study design
A retrospective cohort study was performed in an urban, safety net and tertiary referral medical center over a five-year period. Adult patients undergoing cancer operations were stratified as EP and LEP. We evaluated 30-day revisit to the ED, length of stay (LOS), long-term all-cause mortality, and any major complication on index admission. Regression was used to adjust for baseline comorbidities, case risk, and socioeconomic factors.
Results
A total of 2467 patients were included. There was no difference in case risk between language groups, but EP had a larger proportion of high comorbidity scores. Patients in the non-English group were more likely to be uninsured/self-pay and live in neighborhoods with lower median income. After adjustment, we found no difference in long-term mortality [hazard ratio: 0.87 (95% CI 0.52–1.45)]. LEP patients had the same LOS compared to primary EP patients with an IRR of 0.99 (95% CI 0.88–1.10). There was no difference in the odds of revisit to hospital for LEP versus EP, with an OR of 1.08, 95% CI [0.75–1.53] and no difference in major complication (OR 0.76 (95% CI 0.39–1.45).
Conclusions
We found no association between language and outcomes after cancer operations. This lack of difference may reflect local efficacy at treating non-English-speaking patients, and health systems with fewer services for LEP patients might show different results.


Similar content being viewed by others
References
US Census Bureau. Available at: https://www.census.gov/data/tables/2013/demo/2009-2013-lang-tables.html. Accessed May 23, 2019
Angela Potter-Collins. 2013. Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/language/articles/languageinenglandandwales/2013-03-04#main-language-in-england-and-wales
Hasnain-Wynia R, Yonek J, Pierce D et al. Hospital language services for patients with limited english proficiency: results from a national survey. American Hospital Association: Heatlh Res Edu Trust, 28
Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O (2003) Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep 118:293–302
John-Baptiste A, Naglie G, Tomlinson G et al (2004) The effect of English language proficiency on length of stay and in-hospital mortality. J Gen Intern Med 19:221–228
Ngai KM, Grudzen CR, Lee R et al (2016) The association between limited english proficiency and unplanned emergency department revisit within 72 hours. Ann Emerg Med 68:213–221
Sarver J, Baker DW (2000) Effect of language barriers on follow-up appointments after an emergency department visit. J Gen Intern Med 15:256–264
Carrasquillo O, Orav EJ, Brennan TA, Burstin HR (1999) Impact of language barriers on patient satisfaction in an emergency department. J Gen Intern Med 14:82–87
Feeney T, Cassidy M, Tripodis Y et al (2019) Association of primary language with outcomes after operations typically performed to treat cancer: analysis of a statewide database. Ann Surg Oncol 26:2684–2693
Boston Medical Center. Available at: https://www.bmc.org/about-us
VanderWeele TJ. Principles of confounder selection. [Internet].European journal of epidemiology [Internet].; 2019. Available at: https://link.springer.com/10.1007/s10654-019-00494-6. Accessed March 9, 2019
Harrell Jr FE, Dupont C. Hmisc: Harrell Miscellaneous. 2017. https://CRAN.R-project.org/package=Hmisc
Hadley Wickham. 2017. Tidyverse: Easily Install and Load “Tidyverse” Packages. https://CRAN.Rproject.org/package=tidyverse
Warnes GR, Bolker B, Lumley T, Johnson RC. Gmodels: various R Programming tools for model fitting. [Internet]. In: 2018. Available at: https://CRAN.R-project.org/package=gmodels
Kassambara A, Kosinski M, Biecek P. survminer: Drawing survival curves using “ggplot2”. [Internet]. In: 2017. Available at: https://CRAN.R-project.org/package=survminer
Paredes AZ, Idrees JJ, Beal EW et al (2018) Influence of english proficiency on patient-provider communication and shared decision-making. Surgery 163:1220–1225
Karliner LS, Jacobs EA, Chen AH, Mutha S (2007) Do professional interpreters improve clinical care for patients with limited ENGLISH proficiency? A systematic review of the literature. Health Serv Res 42:727–754
Inagaki E, Farber A, Kalish J et al (2017) Role of language discordance in complication and readmission rate after infrainguinal bypass. J Vasc Surg 66:1473–1478
Grubbs V, Bibbins-Domingo K, Fernandez A et al (2008) Acute myocardial infarction length of stay and hospital mortality are not associated with language preference. J Gen Intern Med 23:190–194
Karliner LS, Kim SE, Meltzer DO, Auerbach AD (2010) Influence of language barriers on outcomes of hospital care for general medicine inpatients. J Hosp Med 5:276–282
Feeney T, Sanchez SE, Tripodis Y et al (2019) The association of primary language with emergency general surgery outcomes using a statewide database. J Surg Res 244:484–491
Clapp B, Jarmillo M, Vigil V et al (2007) Patient comprehension and recall of laparoscopic surgery and outcomes in a non-english speaking population. J Soc Laparoendosc Surg 11(2):242
Mehta SJ (2015) Patient satisfaction reporting and its implications for patient care. AMA J Ethics 17:616–621
Petrullo KA, Lamar S, Nwankwo-Otti O et al (2012) The patient satisfaction survey: what does it mean to your bottom line? J Hosp Adm 2(1):8
Funding
This study was not funded by external funds of grants and was supported solely by internal departmental funds.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JFT is on the board of Mauna Kea Technologies and owns stocks in that company. No other authors have conflicts to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Feeney, T., Park, C., Godley, F. et al. Provider–patient Language Discordance and Cancer Operations: Outcomes from a Single Center Linked to a State Vital Statistics Registry. World J Surg 44, 3324–3332 (2020). https://doi.org/10.1007/s00268-020-05614-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05614-y