Abstract
Background
The aims of the present systematic review and meta-analysis were to compare non-mesh Desarda technique with standard mesh-based Lichtenstein technique for inguinal hernia repair.
Methods
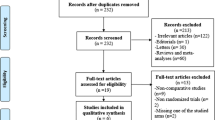
A systematic literature search for RCTs comparing between DT and LT was conducted using electronic databases and Google scholar service. Studies were evaluated for recurrence and post-operative complications. We pooled the data using fixed effects model and random effects model after assessing the heterogeneity among the included studies.
Results
A total number of 8 RCTs studies were included in this meta-analysis with total number of 3177 patients divided between Desarda group and Lichtenstein group as follows: 1551 patients and 1,626 patients, respectively. There was no difference in terms of recurrence between the Desarda repair and Lichtenstein repair groups [P = 0.44]. There was a lower rate of overall post-operative complications [P = 0.003], seroma [P = 0.0004] and surgical site infections (SSIs) [P = 0.04] in the Desarda group.
Conclusion
DT and LT were found to have comparable results in terms of recurrence rate, haematoma formation, testicular atrophy and time to return to normal daily activity/work. DT is superior to LT in terms of reducing post-operative mesh-attributed complications, such as SSI and Seroma formation.










Similar content being viewed by others
References
Primatesta P, Goldacre MJ (1996) Inguinal hernia repair: incidence of elective and emergency surgery, readmission and mortality. Int J Epidemiol 25:835–839
Courtney M, Townsend JR, Beauchamp RD, Evers BM, Mattox KL (2007) In: Courtney M, Townsend JR, Beauchamp RD, Evers BM, Mattox KL (eds) Sabiston textbook of surgery: the biological basis of modern surgical practice, 17th edn. Elsevier Inc, Amsterdam
Vrijland WW, Van Den Tol MP, Luijendijk RW et al (2002) Randomized clinical trial of non-mesh versus mesh repair of primary inguinal hernia. Br J Surg 89:293–297
McRoy LL (2010) Plugoma and the prolene hernia system. J Am Coll Surg 212:424–425
Ahmad MH, Pathak S, Clement KD, Aly EH (2019) Meta-analysis of the use of sterilized mosquito net mesh for inguinal hernia repair in less economically developed countries. BJS Open 3:429–435
Fawole AS, Chaparala RPC, Ambrose NS (2006) Fate of the inguinal hernia following removal of infected prosthetic mesh. Hernia 10:58–61
Genc V, Ensari C, Ergul Z et al (2010) A very late-onset deep infection after prosthetic inguinal hernia repair. Chirurgia (Bucur) 105:555–557
Scott NW, McCormack K, Graham P et al (2002) Open mesh versus non-mesh for repair of femoral and inguinal hernia. Cochrane Database Syst Rev. 2002(4):CD002197. https://doi.org/10.1002/14651858.CD002197
Desarda MP (2006) Physiological repair of inguinal hernia: a new technique (study of 860 patients). Hernia 10:143–146
Desarda M, Ghosh A (2006) Comparative study of open mesh repair and Desarda’s non-mesh repair in a district hospital in India. East Central Afr J Surg 11(2):28–34
Desarda MP (2003) Surgical physiology of inguinal hernia repair—a study of 200 cases. BMC Surgery 3:2. https://doi.org/10.1186/1471-2482-3-2
Higgins JPT, Green S (eds). Cochrane handbook for systematic reviews of interventions, version 5.1.0. https://www.cochrane.org/handbook [Accessed 22 Jun 2015]
Moher D, Liberati A, Tetzlaff J, Altman DG (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8:336–341
Higgins JP, Altman DG, Gotzsche PC et al (2011) Cochrane bias methods group; cochrane statistical methods group. the cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMCMed Res Methodol 5:13
Macaskill P, Walter SD, Irwig L (2001) A comparison of methods to detect publication bias in meta-analysis. Stat Med 20:641–654
Higgins JP, Green S (eds) (2011) Chapter 8: assessing risk of bias in included studies. Cochrane handbook for systematic reviews of interventions. Version 5.1.0. http://handbook-5–1.cochrane.org. Accessed 10 Oct 2018
Szopinski J, Dabrowiecki S, Pierscinski S et al (2012) Desarda versus Lichtenstein technique for primary inguinal hernia treatment: 3-year results of a randomized clinical trial. World J Surg 36:984–992. https://doi.org/10.18203/2349-2902.isj20183191
Rodriguez PRL, Gonzàlez OCL, Rocha JS et al (2018) A randomized trial comparing Desarda repair no mesh and Lichtenstein repair for inguinal hernia (A study of 2225 patients). Biomed J Sci Tech Res 6(4):5445–5449
Manyilirah W, Kijjambu S, Upoki A, Kiryabwire J (2012) Comparison of non-mesh (Desarda) and mesh (Lichtenstein) methods for inguinal hernia repair among black African patients: a short-term double-blind RCT. Hernia 16:133–144
Bhatti IA, Ishaqu H, Ahmad Z, Dar UF (2015) Desarda’s versus Lichtenstein technique of hernia repair. Pak J Med Health Sci 9(4):1331–1333
Ahmad I, Dwivedi AC, Srivastava SK et al (2016) A randomized trial comparing Lichenstein and Desarda technique for open inguinal hernia repair: a study of 100 patient. IOSR J Dent Med Sci 15(3):17–20
Azfal RA, Yousaf S (2017) Outcomes of Desarda vs Lichtenstein repair for inguinal hernia in terms of operative time, seroma formation, return to normal activity and cost. Pak J Med Health Sci 11(1):4
Ahmed AE, Ahmed WB, Omar MA, Redwan AA (2018) Desarda versus Lichtenstein repair for inguinal hernia: a randomized, multi-center controlled trial with promising results. Int Surg J 5(8):2723–2726
Youssef T, El-Alfy K, Farid M (2015) Randomized clinical trial of Desarda versus Lichtenstein repair for treatment of primary inguinal hernia. Int J Surg 20:28–34
Zieren J, Beyersdorff D, Beier KM et al (2001) Sexual function and testicular perfusion after inguinal hernia repair with mesh. Am J Surg 181(3):204–206
Kulacoglu H (2011) Current options in inguinal hernia repair in adult patients. Hippokratia 15(3):223–323
Gedam BS, Bansod PV, Kale VB et al (2017) A comparative study of Desarda's technique with Lichtenstein mesh repair in treatment of inguinal hernia: a prospective cohort study. Int J Surg 39:150–155
Jones P, Jones S, Guarnieri F, Moscatelli F, Desarda MP et al (2015) Topic: inguinal hernia—mesh vs non mesh. Hernia 19(1):265–266
Emile SH, Elfeki H (2018) Desarda’s technique versus Lichtenstein technique for the treatment of primary inguinal hernia: a systematic review and meta-analysis of randomized controlled trials. Hernia 22(3):385–395
Bracale U, Melillo P, Piaggio D et al (2019) Is Shouldice the best NON-MESH inguinal hernia repair technique? A systematic review and network metanalysis of randomized controlled trials comparing Shouldice and Desarda. International Journal of Surgery 62:12–21
Hay JM, Boudet MJ, Fingerhut A et al (1995) Shouldice inguinal hernia repair in the male adult: the gold standard? A multicentral controlled trial in 1578 patients. Ann Surg 222:719–727
Shouldice EB (2003) The Shouldice repair for groin hernias. Surg Clin North Am 83:1163–1187
Junge K, Rosch R, Klinge U et al (2006) Risk factors related to recurrence in inguinal hernia repair: a retrospective analysis. Hernia 10:309–315
Sachs M, Damm M, Encke A (2007) Historical evolution of inguinal hernia repair. World J Surg 21:218–223. https://doi.org/10.5772/58533
Cihan A, Ozdemir H, Uçan BH et al (2006) Fade or fate. Seroma in laparoscopic inguinal hernia repair. Surg Endosc 20(2):325–328
Lehr SC, Schuricht AL (2001) A minimally invasive approach for treating postoperative seromas after incisional hernia repair. JSLS 5(3):267–271
Kapiris SA, Brough WA, Royston CM et al (2001) Laparoscopic transabdominal preperitoneal (TAPP) hernia repair: a 7-year two-center experience in 3017 patients. Surg Endosc 15(9):972–975
Fitzgibbons RJ Jr, Camps J, Cornet DA et al (1995) Laparoscopic inguinal herniorrhaphy: results of a multicenter trial. Ann Surg 221(1):3–13
Falagas ME, Kasiakou SK (2005) Mesh-related infections after hernia repair surgery. Clin Microbiol Infect 11:3–8
Yerdel MA, Akin EB, Dolalan S et al (2001) Effect of single-dose prophylactic ampicillin and sulbactam on wound infection after tension-free inguinal hernia repair with polypropylene mesh: the randomized, double-blind, prospective trial. Ann Surg 233:26–33
Celdran A, Frieyro O, De La Pinta JC et al (2004) The role of antibiotic prophylaxis on wound infection after mesh hernia repair under local anesthesia on an ambulatory basis. Hernia J Hernias Abdom Wall Surg 8:20–22
Musella M, Guido A, Musella S (2001) Collagen tampons as aminoglycoside carriers to reduce postoperative infection rate in prosthetic repair of groin hernias. Eur J Surg Acta Chir 167:130–132
Ge H, Liang C, Xu Y et al (2018) Desarda versus Lichtenstein technique for the treatment of primary inguinal hernia: a systematic review. Int J Surg 50:22–27
Schumpelick V, Fitzgibbons RJ (2007) The mesh and the spermatic cord. Springer, Recurrent Hernia. Heidelberg, pp 333–337
Lee SL, DuBois JJ, Rishi M (2000) Testicular damage after surgical groin exploration for elective herniorrhaphy. M J Pediatr Surg 35(2):327–330
Jones KR, Burney RE, Peterson M, Christy B (2001) Return to work after inguinal hernia repair. Surgery 129(2):128–135
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mohamedahmed, A.Y.Y., Ahmad, H., Abdelmabod, A.A.N. et al. Non-mesh Desarda Technique Versus Standard Mesh-Based Lichtenstein Technique for Inguinal Hernia Repair: A Systematic Review and Meta-analysis. World J Surg 44, 3312–3321 (2020). https://doi.org/10.1007/s00268-020-05587-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05587-y