Abstract
Background
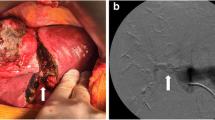
The extrahepatic surgical technique in liver resection can be divided into glissonean pedicle transection and glissonean separated transection approaches. In this study, we compared remnant liver function and liver regeneration involving the Spiegel lobe between these two approaches regarding Spiegel lobe-preserving left hepatectomy.
Methods
We enrolled 31 patients who underwent Spiegel lobe-preserving left hepatectomy for malignant hepatobiliary diseases between April 2008 and January 2020. The postoperative Spiegel lobe volume was measured using a volume analyzer at 3 and 6 months postoperatively.
Results
Of the 31 patients, 22 and 9 were included in the glissonean separated transection and glissonean pedicle transection groups, respectively. There was no significant between-group difference in the preoperative Spiegel lobe volume. However, the volumes at 3 and 6 months postoperatively were significantly larger in the glissonean pedicle transection group than in the glissonean transection group (29.92 mL vs. 13.00 mL; P < 0.001 and 28.43 mL vs. 15.01 mL; P < 0.001, respectively). There was no significant between-group difference in postoperative remnant liver function.
Conclusions
The postoperative Spiegel lobe volume was larger, and liver regeneration was better with the glissonean pedicle transection approach because of transection for Spiegel branch of the portal vein. It is desirable to preserve Spiegel branch in possible cases when surgeons select the glissonean separated transection approach based on the location and size of the tumors.



Similar content being viewed by others
References
Livraghi T, Mäksalo H, Line PD (2011) Treatment options in hepatocellular carcinoma today. Scand J Surg 100:22–29
Rotellar F, Prado F, Benito A, Martí-Cruchaga P, Zozaya G, Pedano N (2012) A novel extra-glissonian approach for totally laparoscopic left hepatectomy. Surg Endosc 26:2617–2622
Couinaud CM (1985) A simplified method for controlled left hepatectomy. Surgery 97:358–361
Takasaki K (1998) Glissonean pedicle transection method for hepatic resection: a new concept of liver segmentation. J Hepatobiliary Pancreat Surg 5:286–291
Ji B, Wang Y, Wang G, Liu Y (2012) Curative resection of hepatocelluar carcinoma using modified glissonean pedicle transection versus the pringle maneuver: a case control study. Int J Med Sci 9:843–852
Cho A, Asano T, Yamamoto H, Nagata M, Takiguchi N, Kainuma O et al (2007) Laparoscopy-assisted hepatic lobectomy using hilar Glissonean pedicle transection. Surg Endosc 21:1466–1468
Lortat-Jacob JL, Robert HG (1952) Well defined technic for right hepatectomy. Presse Med 60:549–551
Honjo I, Araki C (1955) Total resection of the right lobe of the liver; report of a successful case. J Int Coll Surg 23:23–28
Kumon M (2017) Anatomical study of the caudate lobe with special reference to portal venous and biliary branches using corrosion liver casts and clinical application. Liver Cancer 6:161–170
Makuuchi M, Kosuge T, Takayama T, Yamazaki S, Kakazu T, Miyagawa S et al (1993) Surgery for small liver cancers. Semin Surg Oncol 9:298–304
Yoshikawa T, Nomi T, Hokuto D, Yasuda S, Kawaguchi C, Yamada T et al (2017) Risk factors for postoperative ascites in patients undergoing liver resection for hepatocellular carcinoma. World J Surg 41:2095–2100. https://doi.org/10.1007/s00268-017-4003-x
Nomi T, Hokuto D, Yoshikawa T, Matsuo Y, Sho M (2018) A novel navigation for laparoscopic anatomical liver resection using indocyanine green fluorescence. Ann Surg Oncol 25:3982
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L et al (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery 149:680–688
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R et al (2011) Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 149:713–724
Kanda Y (2013) Investigation of the freely avaiable easy-to-use software ' EZR ' for medical statistics. Bone Marrow Transplant 48:452–458
Yamamoto M, Katagiri S, Ariizumi S, Kotera Y, Takahashi Y (2012) Glissonean pedicle transection method for liver surgery (with video). J Hepatobilliary Pancreat Sci 19:3–8
Yang T, Zhang J, Lu JH, Yang GS, Wu MC, Yu WF (2011) Risk factors influencing postoperative outcomes of major hepatic resection of hepatocellular carcinoma for patients with underlying liver diseases. World J Surg 35:2073–2082. https://doi.org/10.1007/s00268-011-1161-0
Fujii M, Shimada M, Satoru I, Morine Y, Ikemoto T, Soejima Y (2007) A standardized safe hepatectomy; selective Glissonean transection using endolinear stapling devices. Hepatogastroenterology 54:906–909
Aoki T, Imamura H, Matsuyama Y, Kishi Y, Kobayashi T, Sugawara Y et al (2011) Convergence process of volumetric liver regeneration after living-donor hepatectomy. J Gastrointest Surg 15:1594–1601
Yamanaka N, Okamoto E, Kawamura E, Kato T, Oriyama T, Fujimoto J et al (1993) Dynamics of normal and injured human liver regeneration after hepatectomy as assessed on the basis of computed tomography and liver function. Hepatology 18:79–85
Truant S, Bouras AF, Petrovai G, Buob D, Ernst O, Boleslawski E et al (2013) Volumetric gain of the liver after major hepatectomy in obese patients: a case-matched study in 84 patients. Ann Surg 258:696–702 discussion 702–4
Yamaguchi T, Kokubo T, Akamatsu N, Kaneko J, Arita J, Sakamoto Y et al (2018) Liver regeneration is preserved after at least four repeated liver resections for hepatocellular carcinoma. World J Surg 42:4070–4080. https://doi.org/10.1007/s00268-018-4714-7
Ibis C, Asenov Y, Akin M, Azamat IF, Sivrikoz N, Gurtekin B (2017) Factors affecting liver regeneration in living donors after hepatectomy. Med Sci Monit 18:5986–5993
Matot I, Nachmansson N, Duev O, Schulz S, Schroeder-Stein K, Frede S et al (2017) Impaired liver regeneration after hepatectomy and bleeding is associated with a shift from hepatocyte proliferation to hypertrophy. FASEB J 31:5283–5295
Acknowledgements
We gratefully acknowledge the work of the past and present members of our division.
Funding
This study did not receive funding from any organization.
Author information
Authors and Affiliations
Contributions
NK conducted the literature search and review, collected data, and drafted the manuscript. TN and DH proofread the manuscript. TY and YM discussed the significance of this manuscript. MS reviewed the manuscript and provided advice regarding the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kamitani, N., Nomi, T., Hokuto, D. et al. Influence of the Glissonean Pedicle Transection Approach in Spiegel Lobe-Preserving Left Hepatectomy on Spiegel Lobe Volume and Remnant Liver Functions. World J Surg 44, 3079–3085 (2020). https://doi.org/10.1007/s00268-020-05548-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05548-5