Abstract
Background
Although bullectomy is the most curative treatment in primary spontaneous pneumothorax (PSP), postoperative recurrence is not uncommon. New bulla formation at the staple line is the most common cause of recurrence. However, the mechanism is not known. We believe that the pressure gradient plays the main role in new bulla formation. A large resection amount induces a prolonged pressure gradient for obliteration of the residual space. This study aimed to identify the association between resected lung volume and recurrence.
Methods
The medical records of patients who underwent video-assisted thoracoscopic surgery (VATS) bullectomy were reviewed between October 2010 and December 2017. A total of 396 patients underwent surgery for spontaneous pneumothorax. The electronic medical records (EMRs) of the patients were reviewed. Patients with secondary spontaneous pneumothorax were excluded. Patients who were diagnosed with emphysema on CT were excluded. Patients with PSP were excluded from the study if the bulla was not located in the apex or if there was no ruptured bulla at the time of the operation. Patients who lacked EMRs were also excluded. We reviewed the medical records of 276 patients. The apical resected lung volume was estimated using a conical volumetric formula with the use of the specimen size. The risk factors for postoperative recurrence were analyzed.
Results
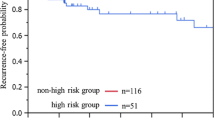
The median age was 19 years old (range 13–36). A total of 261 patients were male (94.6%). The median body weight and body mass index (BMI) were 58 kg (range 40–82) and 18.92 (range 15.21–26.47), respectively. In 24 patients, both sides were operated on simultaneously. The resected lung volume was obtained by using a conical volumetric formula, and the value was divided by the BMI value. The median value was 1.43 (0.03–5.67). The median operative time was 35 min (range 15–120). The median postoperative day was 4 (range 2–12). Age (p = 0.006), the value of the resected lung volume divided by BMI (p = 0.003), bilateral bullectomy (p = 0.013) and transverse diameter (p = 0.034) were associated with postoperative recurrence according to the univariate analysis. According to the multivariate analysis, age and the value of the lung volume divided by BMI were significant risk factors for postoperative recurrence.
Conclusions
Younger age and a large resected lung volume and a low BMI are associated with postoperative recurrence after VATS bullectomy for PSP.


Similar content being viewed by others
References
Sahn SA, Heffner JE (2000) Spontaneous pneumothorax. N Engl J Med 342:868–874
MacDuff A, Arnold A (2010) Harvey J (2010) Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline. Thorax 65:ii18-31
Olesen WH, Lindahl-Jacobsen R, Katballe N et al (2016) Recurrent primary spontaneous pneumothorax is common following chest tube and conservative treatment. World J Surg 40:2163–2170. https://doi.org/10.1007/s00268-016-3508-z
Waller DA, Forty J, Morritt GN (1994) Video-assisted thoracoscopic surgery versus thoracotomy for spontaneous pneumothorax. Ann Thorac Surg 58:372–376
Cho S, Jheon S, Kin DK et al (2018) Results of repeated video-assisted thoracic surgery for recurrent pneumothorax after primary spontaneous pneumothorax. Eur J Cardiothorac Surg 53:857–861
Tsuboshima K, Nagata M, Wakahara T et al (2015) Relationship between postoperative bulla neogenesis at the staple line and the resected lung volume in primary spontaneous pneumothorax. Gen Thorac Cardiovasc Surg 63:572–575
Kenny BJ, Ponichtera K (2019) Physiology, Boyle’s law. StatPearls Publishing, Treasure Island
Jeon HW, Kim YD (2016) Does 11.5 mm guided single port surgery has clinical advantage than multi-port thoracoscopic surgery in spontaneous pneumothorax? J Thorac Dis 8:2924–2930
Athanassiadi K, Kalavrouziotis G, Loutsidis A et al (1998) Surgical treatment of spontaneous pneumothorax: ten-year experience. World J Surg 22:803–806. https://doi.org/10.1007/s002689900473
Delpy JP, Pages PB, Mordant P et al (2016) Surgical management of spontaneous pneumothorax: are there any prognostic factors influencing postoperative complications? Eur J Cardiothorac Surg 49:862–867
Ling ZG, Wu YB, Ming MY et al (2015) The effect of pleural abrasion on the treatment of primary spontaneous pneumothorax: a systematic review of randomized controlled trials. PLoS ONE 10:e0127857
Lang-Lazdunski L, Chapuis O, Bonnet PM et al (2003) Videothoracoscopic bleb excision and pleural abrasion for the treatment of primary spontaneous pneumothorax: long-term results. Ann Thorac Surg 75:960–965
Lee S, Kim HR, Cho S et al (2014) Staple line coverage after bullectomy for primary spontaneous pneumothorax: a randomized trial. Ann Thorac Surg 98:2005–2011
Min X, Huang Y, Yang Y et al (2014) Mechanical pleurodesis does not reduce recurrence of spontaneous pneumothorax: a randomized trial. Ann Thorac Surg 98:1790–1796
Cardillo G, Bintcliffe OJ, Carleo F et al (2016) Primary spontaneous pneumothorax: a cohort study of VATS with talc poudrage. Thorax 71:847–853
Ng C, Maier HT, Kocher F et al (2018) VATS partial pleurectomy versus VATS pleural abrasion: significant reduction in pneumothorax recurrence rates after pleurectomy. World J Surg 42:3256–3262. https://doi.org/10.1007/s00268-018-4640-8
Gaunt A, Martin-Ucar AE, Beggs L et al (2008) Residual apical space following surgery for pneumothorax increases the risk of recurrence. Eur J Cardiothorac Surg 34:169–173
Choi SY, Kim YD, Suh JH et al (2018) New bullae formation in the staple ling increases the risk of recurrent pneumothorax following video-assisted thoracoscopic surgery bullectomy for primary spontaneous pneumothorax. J Thorac Dis 10:4287–4292
Choi SY, Du Kim Y, Kim YD et al (2018) Influence of lung resection volume on risk of primary spontaneous pneumothorax recurrence. J Thorac Dis 10:1622–1627
Tan J, Yang Y, Zhong J et al (2017) Association between BMI and recurrence of primary spontaneous pneumothorax. World J Surg 41:1274–1280. https://doi.org/10.1007/s00268-016-3848-8
Noh D, Lee S, Haam SJ et al (2015) Recurrence of primary spontaneous pneumothorax in young adults and children. Interact Cariovasc Thorac Surg 21:195–199
Hirai K, Kawashima T, Takeuchi S et al (2015) Covering the staple line with a polyglycolic acid sheet after bullectomy for primary spontaneous pneumothorax prevents postoperative recurrent pneumothorax. J Thorac Dis 7:1978–1985
Acknowledgements
This manuscript has been edited by native English-speaking experts of American Journal Experts.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jeon, H.W., Kim, YD. & Sim, S.B. Should We Consider the Resected Lung Volume in Primary Spontaneous Pneumothorax?. World J Surg 44, 2797–2803 (2020). https://doi.org/10.1007/s00268-020-05522-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05522-1