Abstract
Background
Anatomical resection (AR) for colorectal liver metastasis (CLM) is disputable. We investigated the impact of AR on short-term outcomes and survival in CLM patients.
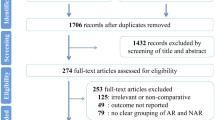
Methods
Patients having hepatectomy with AR or nonanatomical resection (NAR) for CLM were reviewed. Comparison was made between AR and NAR groups. Group comparison was performed again after propensity score matching with ratio 1:1.
Results
AR group (n = 234 vs n = 89 in NAR group) had higher carcinoembryonic antigen level (20 vs 7.8 ng/mL, p ≤ 0.001), more blood loss (0.65 vs 0.2 L, p < 0.001), more transfusions (19.2% vs 3.4%, p = 0.001), longer operation (339.5 vs 180 min, p < 0.001), longer hospital stay (9 vs 6 days, p < 0.001), more tumors (p < 0.001), larger tumors (4 vs 2 cm, p < 0.001), more bilobar involvement (20.9% vs 7.9%, p = 0.006), and comparable survival (overall, p = 0.721; disease-free, p = 0.695). After propensity score matching, each group had 70 patients, with matched tumor number, tumor size, liver function, and tumor marker. AR group had more open resections (85.7% vs 68.6%, p = 0.016), more blood loss (0.556 vs 0.3 L, p = 0.001), more transfusions (17.1% vs 4.3%, p = 0.015), longer operation (310 vs 180 min, p < 0.001), longer hospital stay (8.5 vs 6 days, p = 0.002), comparable overall survival (p = 0.819), and comparable disease-free survival (p = 0.855).
Conclusion
Similar disease-free survival and overall survival of CLM patients were seen with the use of AR and NAR. However, AR may entail a more eventful postoperative course. NAR with margin should be considered whenever feasible.


Similar content being viewed by others
References
Minagawa M, Makuuchi M, Torzilli G, Takayama T, Kawasaki S, Kosuge T et al (2000) Extension of the frontiers of surgical indications in the treatment of liver metastases from colorectal cancer: long-term results. Ann Surg 231(4):487–499
Abdalla EK, Vauthey JN, Ellis LM, Ellis V, Pollock R, Broglio KR et al (2004) Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Ann Surg 239(6):818–825 (discussion 25–27)
Pawlik TM, Scoggins CR, Zorzi D, Abdalla EK, Andres A, Eng C et al (2005) Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg 241(5):715–722 (discussion 22–24)
Spelt L, Andersson B, Nilsson J, Andersson R (2012) Prognostic models for outcome following liver resection for colorectal cancer metastases: a systematic review. Eur J Surg Oncol 38(1):16–24
Zorzi D, Laurent A, Pawlik TM, Lauwers GY, Vauthey JN, Abdalla EK (2007) Chemotherapy-associated hepatotoxicity and surgery for colorectal liver metastases. Brit J Surg 94(3):274–286
Vauthey JN, Pawlik TM, Ribero D, Wu TT, Zorzi D, Hoff PM et al (2006) Chemotherapy regimen predicts steatohepatitis and an increase in 90-day mortality after surgery for hepatic colorectal metastases. J Clin Oncol 24(13):2065–2072
Lalmahomed ZS, Ayez N, van der Pool AE, Verheij J, Joanne IJ, Verhoef C (2011) Anatomical versus nonanatomical resection of colorectal liver metastases: is there a difference in surgical and oncological outcome? World J Surg 35(3):656–661. https://doi.org/10.1007/s00268-010-0890-9
Stewart GD, O’Suilleabhain CB, Madhavan KK, Wigmore SJ, Parks RW, Garden OJ (2004) The extent of resection influences outcome following hepatectomy for colorectal liver metastases. Eur J Surg Oncol 30(4):370–376
Sarpel U, Bonavia AS, Grucela A, Roayaie S, Schwartz ME, Labow DM (2009) Does anatomic versus nonanatomic resection affect recurrence and survival in patients undergoing surgery for colorectal liver metastasis? Ann Surg Oncol 16(2):379–384
Kokudo N, Tada K, Seki M, Ohta H, Azekura K, Ueno M et al (2001) Anatomical major resection versus nonanatomical limited resection for liver metastases from colorectal carcinoma. Am J Surg 181(2):153–159
Yamamoto J, Kosuge T, Shimada K, Yamasaki S, Moriya Y, Sugihara K (1999) Repeat liver resection for recurrent colorectal liver metastases. Am J Surg 178(4):275–281
Shaw IM, Rees M, Welsh FK, Bygrave S, John TG (2006) Repeat hepatic resection for recurrent colorectal liver metastases is associated with favourable long-term survival. Brit J Surg 93(4):457–464
Petrowsky H, Gonen M, Jarnagin W, Lorenz M, DeMatteo R, Heinrich S et al (2002) Second liver resections are safe and effective treatment for recurrent hepatic metastases from colorectal cancer: a bi-institutional analysis. Ann Surg 235(6):863–871
Fan ST (2010) Liver functional reserve estimation: state of the art and relevance for local treatments: the Eastern perspective. J Hepatobiliary Pancreat Surg 17(4):380–384
Chan SC, Liu CL, Lo CM, Lam BK, Lee EW, Wong Y et al (2006) Estimating liver weight of adults by body weight and gender. World J Gastroenterol 12(14):2217–2222
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Edge S, Byrd DR, Compton CC, Fritz AG, Greene F, Trotti A (eds) (2010) AJCC cancer staging manual, 7th edn. Springer, New York
Cheung TT, Poon RT, Dai WC, Chok KS, Chan SC, Lo CM (2016) Pure laparoscopic versus open left lateral sectionectomy for hepatocellular carcinoma: a single-center experience. World J Surg 40(1):198–205. https://doi.org/10.1007/s00268-015-3237-8
Cheung TT, Poon RT, Yuen WK, Chok KS, Tsang SH, Yau T et al (2013) Outcome of laparoscopic versus open hepatectomy for colorectal liver metastases. ANZ J Surg 83(11):847–852
Terminology Committee of the IHPBA (2000) Terminology of liver anatomy and resections. HPB Surg 2:333–339
Ueno S, Kubo F, Sakoda M, Hiwatashi K, Tateno T, Mataki Y et al (2008) Efficacy of anatomic resection vs nonanatomic resection for small nodular hepatocellular carcinoma based on gross classification. J Hepatobiliary Pancreat Surg 15(5):493–500
Wakai T, Shirai Y, Sakata J, Kaneko K, Cruz PV, Akazawa K et al (2007) Anatomic resection independently improves long-term survival in patients with T1–T2 hepatocellular carcinoma. Ann Surg Oncol 14(4):1356–1365
Hasegawa K, Kokudo N, Imamura H, Matsuyama Y, Aoki T, Minagawa M et al (2005) Prognostic impact of anatomic resection for hepatocellular carcinoma. Ann Surg 242(2):252–259
Chen J, Huang K, Wu J, Zhu H, Shi Y, Wang Y et al (2011) Survival after anatomic resection versus nonanatomic resection for hepatocellular carcinoma: a meta-analysis. Dig Dis Sci 56(6):1626–1633
Cucchetti A, Cescon M, Ercolani G, Bigonzi E, Torzilli G, Pinna AD (2012) A comprehensive meta-regression analysis on outcome of anatomic resection versus nonanatomic resection for hepatocellular carcinoma. Ann Surg Oncol 19(12):3697–3705
DeMatteo RP, Palese C, Jarnagin WR, Sun RL, Blumgart LH, Fong Y (2000) Anatomic segmental hepatic resection is superior to wedge resection as an oncologic operation for colorectal liver metastases. J Gastrointest Surg 4(2):178–184
Finch RJ, Malik HZ, Hamady ZZ, Al-Mukhtar A, Adair R, Prasad KR et al (2007) Effect of type of resection on outcome of hepatic resection for colorectal metastases. Brit J Surg 94(10):1242–1248
Guzzetti E, Pulitano C, Catena M, Arru M, Ratti F, Finazzi R et al (2008) Impact of type of liver resection on the outcome of colorectal liver metastases: a case-matched analysis. J Surg Oncol 97(6):503–507
Tang H, Li B, Zhang H, Dong J, Lu W (2016) Comparison of anatomical and nonanatomical hepatectomy for colorectal liver metastasis: a meta-analysis of 5207 patients. Sci Rep 6:32304
de Haas RJ, Wicherts DA, Flores E, Azoulay D, Castaing D, Adam R (2008) R1 resection by necessity for colorectal liver metastases: is it still a contraindication to surgery? Ann Surg 248(4):626–637
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH (1999) Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 230(3):309–318 (discussion 18–21)
Nordlinger B, Guiguet M, Vaillant JC, Balladur P, Boudjema K, Bachellier P et al (1996) Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1568 patients. Association Francaise de Chirurgie. Cancer 77(7):1254–1262
Rees M, Tekkis PP, Welsh FK, O’Rourke T, John TG (2008) Evaluation of long-term survival after hepatic resection for metastatic colorectal cancer: a multifactorial model of 929 patients. Ann Surg 247(1):125–135
Tanaka K, Shimada H, Ueda M, Matsuo K, Endo I, Togo S (2007) Long-term characteristics of 5-year survivors after liver resection for colorectal metastases. Ann Surg Oncol 14(4):1336–1346
Wei AC, Greig PD, Grant D, Taylor B, Langer B, Gallinger S (2006) Survival after hepatic resection for colorectal metastases: a 10-year experience. Ann Surg Oncol 13(5):668–676
Cata JP, Chukka V, Wang H, Feng L, Gottumukkala V, Martinez F et al (2013) Perioperative blood transfusions and survival in patients with non-small cell lung cancer: a retrospective study. BMC Anesthesiol 13(1):42
Lyu X, Qiao W, Li D, Leng Y (2017) Impact of perioperative blood transfusion on clinical outcomes in patients with colorectal liver metastasis after hepatectomy: a meta-analysis. Oncotarget 8(25):41740–41748
Farid SG, Aldouri A, Morris-Stiff G, Khan AZ, Toogood GJ, Lodge JP et al (2010) Correlation between postoperative infective complications and long-term outcomes after hepatic resection for colorectal liver metastasis. Ann Surg 251(1):91–100
Laurent C, Sa Cunha A, Couderc P, Rullier E, Saric J (2003) Influence of postoperative morbidity on long-term survival following liver resection for colorectal metastases. Brit J Surg 90(9):1131–1136
Shirai Y, Wakai T, Ohtani T, Sakai Y, Tsukada K, Hatakeyama K (1996) Colorectal carcinoma metastases to the liver. Does primary tumor location affect its lobar distribution? Cancer 77(11):2213–2216
Ciliberto D, Prati U, Roveda L, Barbieri V, Staropoli N, Abbruzzese A et al (2012) Role of systemic chemotherapy in the management of resected or resectable colorectal liver metastases: a systematic review and meta-analysis of randomized controlled trials. Oncol Rep 27(6):1849–1856
Cossu ML, Ginesu GC, Feo CF, Fancellu A, Pinna A, Vargiu I et al (2017) Surgical outcomes in patients with hepatic synchronous and metachronous colorectal metastases. Ann Ital Chir 88:497–504
Adson MA, van Heerden JA, Adson MH, Wagner JS, Ilstrup DM (1984) Resection of hepatic metastases from colorectal cancer. Arch Surg 119(6):647–651
Scheele J, Altendorf-Hofmann A (1999) Resection of colorectal liver metastases. Langenbeck’s Arch Surg 384(4):313–327
Tsai MS, Su YH, Ho MC, Liang JT, Chen TP, Lai HS et al (2007) Clinicopathological features and prognosis in resectable synchronous and metachronous colorectal liver metastasis. Ann Surg Oncol 14(2):786–794
van der Pool AE, Lalmahomed ZS, Ozbay Y, de Wilt JH, Eggermont AM, Jzermans JN et al (2010) ‘Staged’ liver resection in synchronous and metachronous colorectal hepatic metastases: differences in clinicopathological features and outcome. Colorectal Dis 12(10 Online):e229–e235
Bockhorn M, Frilling A, Fruhauf NR, Neuhaus J, Molmenti E, Trarbach T et al (2008) Survival of patients with synchronous and metachronous colorectal liver metastases—is there a difference? J Gastrointest Surg 12(8):1399–1405
Allard MA, Cunha AS, Gayet B, Adam R, Goere D, Bachellier P et al (2015) Early and long-term oncological outcomes after laparoscopic resection for colorectal liver metastases: a propensity score-based analysis. Ann Surg 262(5):794–802
Ratti F, Catena M, Di Palo S, Staudacher C, Aldrighetti L (2015) Laparoscopic approach for primary colorectal cancer improves outcome of patients undergoing combined open hepatic resection for liver metastases. World J Surg 39(10):2573–2582. https://doi.org/10.1007/s00268-015-3127-0
Beppu T, Wakabayashi G, Hasegawa K, Gotohda N, Mizuguchi T, Takahashi Y et al (2015) Long-term and perioperative outcomes of laparoscopic versus open liver resection for colorectal liver metastases with propensity score matching: a multi-institutional Japanese study. J Hepatobiliary Pancreat Surg 22(10):711–720
Fretland AA, Kazaryan AM, Bjornbeth BA, Flatmark K, Andersen MH, Tonnessen TI et al (2015) Open versus laparoscopic liver resection for colorectal liver metastases (the Oslo-CoMet Study): study protocol for a randomized controlled trial. Trial. 16:73
Hasegawa Y, Nitta H, Sasaki A, Takahara T, Itabashi H, Katagiri H et al (2015) Long-term outcomes of laparoscopic versus open liver resection for liver metastases from colorectal cancer: a comparative analysis of 168 consecutive cases at a single center. Surgery 157(6):1065–1072
Choi Y, Han HS, Sultan AM, Yoon YS, Cho JY (2014) Glissonean pedicle approach in laparoscopic anatomical liver resection. Hepatogastroenterology 61(136):2317–2320
Ikeda T, Toshima T, Harimoto N, Yamashita Y, Ikegami T, Yoshizumi T et al (2014) Laparoscopic liver resection in the semiprone position for tumors in the anterosuperior and posterior segments, using a novel dual-handling technique and bipolar irrigation system. Surg Endosc 28(8):2484–2492
Lee W, Han HS, Yoon YS, Cho JY, Choi Y, Shin HK (2014) Role of intercostal trocars on laparoscopic liver resection for tumors in segments 7 and 8. J Hepatobiliary Pancreat Surg 21(8):E65–E68
Ishizawa T, Gumbs AA, Kokudo N, Gayet B (2012) Laparoscopic segmentectomy of the liver: from segment I to VIII. Ann Surg 256(6):959–964
Vibert E, Kouider A, Gayet B (2004) Laparoscopic anatomic liver resection. HPB 6(4):222–229
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any conflict of interest.
Ethical approval
Institution research ethics committee approval was not needed for retrospective study of anonymous clinical data.
Informed consent
Informed consent to the study from patients was not needed as it is a review and analysis of anonymous clinical data and no individuals can be identified by the reported data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
She, W.H., Cheung, T.T., Ma, K.W. et al. Anatomical Versus Nonanatomical Resection for Colorectal Liver Metastasis. World J Surg 44, 2743–2751 (2020). https://doi.org/10.1007/s00268-020-05506-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05506-1