Abstract
Background
Pre-incision wound infiltration using NSAID is an alternative method to manage post-operative pain in surgery. It is postulated that NSAID delivered peripherally exerts efficient analgesic and anti-inflammatory effect with minimal systemic complication. This study explored the efficacy of using diclofenac for wound infiltration in open thyroidectomy and parathyroidectomy as compared to conventional agent, bupivacaine.
Methodology
The study was designed as a double-blind, randomized controlled trial involving 94 patients who underwent open thyroidectomy or parathyroidectomy in Hospital Pulau Pinang, Malaysia, from November 2015 to November 2016. The study compared the efficacy of pre-incision wound infiltration of diclofenac (n = 47) versus bupivacaine (n = 47) in post-operative pain relief. Wound infiltration is given prior to skin incision. Mean pain score at designated time interval within the 24-h post-operative period, time to first analgesia, total analgesic usage and total analgesic cost were assessed.
Results
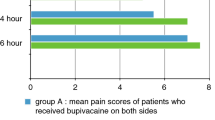
Ninety-four patients were recruited with no dropouts. Mean age was 49.3 (SD = 14.2) with majority being female (74.5%). Ethnic distribution recorded 42.6% Chinese, 38.3% Malay, followed by 19.1% Indian. Mean duration of surgery was 123.8 min (SD = 56.5), and mean length of hospital stay was 4.7 days (SD = 1.8). The characteristics of patient in both groups were generally comparable except that there were more cases of total thyroidectomy in the diclofenac group (n = 31) as compared to the bupivacaine group (n = 16). Mean pain score peaked at immediate post-operative period (post-operative 0.5 h) with a score of 3.5 out of 10 and the level decreased steadily over the next 20 h starting from 4 h post-operatively. Pre-incision wound infiltration using diclofenac had better pain control as compared to bupivacaine at all time interval assessed. In the resting state, the mean post-operative pain score difference was statistically significant at 2 h [2.1 (SD = 1.5) vs. 2.8 (SD = 1.8), p = 0.04]. During neck movement, the dynamic pain score difference was statistically significant at post-operative 1 h [2.7 (SD = 1.9) vs. 3.7 (SD = 2.1), p = 0.02]; 2 h [2.7 (SD = 1.6) vs. 3.7 (SD = 2.0), p = 0.01]; 4 h [2.2 (SD = 1.5) vs. 2.9 (SD = 1.7), p = 0.04], 6 h [1.9 (SD = 1.4) vs. 2.5 (SD = 1.6), p = 0.04] and 12 h [1.5 (SD = 1.5) vs. 2.2 (SD = 1.4), p = 0.03]. Mean dose of tramadol used as rescue analgesia in 24 h duration was lower in the diclofenac group as compared to bupivacaine group [13.8 mg (SD = 24.9) vs. 36.2 mg (SD = 45.1), p = 0.01]. The total cost of analgesia used was significantly cheaper in diclofenac group as compared to bupivacaine group [RM 3.47 (SD = 1.51) vs. RM 13.43 (SD = 1.68), p < 0.01] or [USD 0.83 (SD = 0.36) vs. USD 3.21 (SD = 0.40), p < 0.01].
Conclusion
Pre-incision wound infiltration using diclofenac provides better post-operative pain relief compared to bupivacaine for patient who had underwent open thyroidectomy or parathyroidectomy. Diclofenac is cheap and easily available in the limited resource setting. This approach offers a superior alternative for post-operative pain relief as compared to bupivacaine.





Similar content being viewed by others
References
Aysenur D, Ali A, Mine C, Mehmet A, Ilker I, Ekinci M, Haci Ahmet A (2014) Which method is the most effective for reducing post-thyroidectomy pain: bilateral superficial cervical block or wound infiltration? A prospective randomized, double-blind study. Acta Med Mediterr 30:1159–1164
Dieudonne N, Gomola A, Bonnichon P, Ozier YM (2001) Prevention of postoperative pain after thyroid surgery: a double-blind randomized study of bilateral superficial cervical plexus blocks. Anesth Analg 92(6):1538–1542. https://doi.org/10.1097/00000539-200106000-00038
Kalmovich LM, Cote V, Sands N, Black M, Payne R, Hier M (2010) Thyroidectomy: exactly how painful is it? J Otolaryngol Head Neck Surg 39(3):277–283. https://doi.org/10.2310/7070.2009.090167
Karamanlioglu B, Turan A, Memis D, Kaya G, Ozata S, Ture M (2005) Infiltration with ropivacaine plus lornoxicam reduces postoperative pain and opioid consumption. Can J Anaesth 52(10):1047–1053. https://doi.org/10.1007/BF03021603
Motamed C, Merle JC, Yakhou L, Combes X, Vodinh J, Kouyoumoudjian C, Duvaldestin P (2006) Postoperative pain scores and analgesic requirements after thyroid surgery: comparison of three intraoperative opioid regimens. Int J Med Sci 3(1):11–13. https://doi.org/10.7150/ijms.3.11
Defechereux T, Meurisse M, Hamoir E, Gollogly L, Joris J, Faymonville ME (1999) Hypnoanesthesia for endocrine cervical surgery: a statement of practice. J Altern Complement Med 5(6):509–520. https://doi.org/10.1089/acm.1999.5.509
Park GR, Drummond GB, Sinclair IS, Peck DF (1983) Bupivacaine infiltration for thyroid surgery. J R Coll Surg Edinb 28(5):295–296
Trottier DC, Barron P, Moonje V, Tadros S (2009) Outpatient thyroid surgery: Should patients be discharged on the day of their procedures? Can J Surg 52(3):182–186
Viswanathan K, Manjusha V, Jithunath M (2015) Daycare thyroid surgery: can it be a reality? Int Surg J 2(1):5
Lee SY, Lee WH, Lee EH, Han KC, Ko YK (2010) The effects of paracetamol, ketorolac, and paracetamol plus morphine on pain control after thyroidectomy. Korean J Pain 23(2):124–130. https://doi.org/10.3344/kjp.2010.23.2.124
MOH/P/PAK/257.12 (HB) Pain Management Handbook, 2013
Ramsay MAE (2000) Acute postoperative pain management. Proceedings (Baylor University. Medical Center) 13(3):244–247
Hanna MN, Murphy JD, Kumar K, Wu CL (2009) Regional techniques and outcome: what is the evidence? Curr Opin Anaesthesiol 22(5):672–677. https://doi.org/10.1097/ACO.0b013e32832f330a
Warschkow R, Tarantino I, Jensen K, Beutner U, Clerici T, Schmied BM, Steffen T (2012) Bilateral superficial cervical plexus block in combination with general anesthesia has a low efficacy in thyroid surgery: a meta-analysis of randomized controlled trials. Thyroid 22(1):44–52. https://doi.org/10.1089/thy.2011.0260
Kvolik S, Kristek J, Sakic L, Takač I, Gulam D (2009) A wound infiltration as a method of postoperative analgesia. Periodicum Biologorum 111(2):111
Scott NB (2010) Wound infiltration for surgery. Anaesthesia 65(Suppl 1):67–75. https://doi.org/10.1111/j.1365-2044.2010.06241.x
Gozal Y, Shapira SC, Gozal D, Magora F (1994) Bupivacaine wound infiltration in thyroid surgery reduces postoperative pain and opioid demand. Acta Anaesthesiol Scand 38(8):813–815
Alsaif AAN, Nawaz S, Alotaibi W (2004) Effect of pre-emptive bupivacaine infiltration on post thyroidectomy pain. Internet J Anesthesiol 9:1
Kelly DJ, Ahmad M, Brull SJ (2001) Preemptive analgesia I: physiological pathways and pharmacological modalities. Can J Anaesth 48(10):1000–1010. https://doi.org/10.1007/BF03016591
Kelly DJ, Ahmad M, Brull SJ (2001) Preemptive analgesia II: recent advances and current trends. Can J Anaesth 48(11):1091–1101. https://doi.org/10.1007/BF03020375
Chou F-F, Yang LC, Buerkle H (1999) Effect of pre-incisional versus post-incisional infiltration of lidocaine in patients undergoing thyroid surgery. Acute Pain 2(2):73–78. https://doi.org/10.1016/S1366-0071(99)80042-4
Ekinci MGB, Yeksan AN, Dülgeroğlu O, Aksun M, Baysal PK (2017) Comparison of preincisional and postincisional 0.25% levobupivacaine infiltration in thyroid surgery. J Clin Anal Med 8(1):74–77
Kissin I (2009) Pre-emptive analgesia. Anesthesiology 93:1138–1143
Vadivelu N, Mitra S, Schermer E, Kodumudi V, Kaye AD, Urman RD (2014) Preventive analgesia for postoperative pain control: a broader concept. Local Reg Anesth 7:17–22. https://doi.org/10.2147/LRA.S62160
Dumlu EG, Tokaç M, Öcal H, Durak D, Kara H, Kılıç M, Yalçın A (2016) Local bupivacaine for postoperative pain management in thyroidectomized patients: a prospective and controlled clinical study. Turkish J Surg 32(3):173–177. https://doi.org/10.5152/UCD.2015.3138
Teksoz S, Arikan AE, Soylu S, Erbabacan SE, Ozcan M, Bukey Y (2016) Bupivacaine application reduces post thyroidectomy pain: Cerrahpasa experience. Gland Surg 5(6):565–570. https://doi.org/10.21037/gs.2016.12.04
Ayman MMG, Bericotti M, Rago R, Nidal Y, Miccoli P (2012) Bupivacaine 0.5% versus ropivacaine 0.75% wound infiltration to decrease postoperative pain in total thyroidectomy, a prospective controlled study. Minerva Chir 67(6):511–516
Burian M, Geisslinger G (2005) COX-dependent mechanisms involved in the antinociceptive action of NSAIDs at central and peripheral sites. Pharmacol Ther 107(2):139–154. https://doi.org/10.1016/j.pharmthera.2005.02.004
Romsing J, Moiniche S, Ostergaard D, Dahl JB (2000) Local infiltration with NSAIDs for postoperative analgesia: evidence for a peripheral analgesic action. Acta Anaesthesiol Scand 44(6):672–683
Romsing J, Mysager S, Vilmann P, Sonne J, Larsen NE, Stergaard D (2001) Postoperative analgesia is not different after local vs systemic administration of meloxicam in patients undergoing inguinal hernia repair. Can J Anaesth 48(10):978–984
Lavand'homme PM, Roelants F, Waterloos H, De Kock MF (2007) Postoperative analgesic effects of continuous wound infiltration with diclofenac after elective cesarean delivery. Anesthesiology 106(6):1220–1225. https://doi.org/10.1097/01.anes.0000267606.17387.1d
Lin CF, Wong KL, Chan YL, Wang JM, Wu KH, Wei TT (1998) Comparison of local infiltration of tenoxicam and intravenous tenoxicam for postoperative analgesia in herniorrhaphy. Acta Anaesthesiol Sin 36(1):23–29
Connelly NR, Reuben SS, Albert M, Page D (1997) Use of preincisional ketorolac in hernia patients: intravenous versus surgical site. Reg Anesth 22(3):229–232
Kardash KJ, Garzon J, Velly AM, Tessler MJ (2005) Ketorolac analgesia for inguinal hernia repair is not improved by peripheral administration. Can J Anaesth 52(6):613–617
Marbaix CRF, Mercier V, Waterloos H, Lacrosse D, Lavand’homme P (2004) Post cesarean section analgesia with continuous local infusion of ropivacaine or diclofenac. Int J Obstetric Anesth 13:S1–S40
Toms L, McQuay HJ, Derry S, Moore RA (2008) Single dose oral paracetamol (acetaminophen) for postoperative pain in adults. Cochrane Database Syst Review 2008(4):CD04602. https://doi.org/10.1002/14651858.CD004602.pub2
Ong CK, Seymour RA, Lirk P, Merry AF (2010) Combining paracetamol (acetaminophen) with nonsteroidal antiinflammatory drugs: a qualitative systematic review of analgesic efficacy for acute postoperative pain. Anesth Analg 110(4):1170–1179. https://doi.org/10.1213/ANE.0b013e3181cf9281
Chapman PJ (1987) Review: bupivacaine—a long-acting local anaesthetic. Aust Dent J 32(4):288–291
Davies NM, Anderson KE (1997) Clinical Pharmacokinetics of Diclofenac. Therapeutic insights and pitfalls. Clin Pharmacokinetic 33:184
Gan TJ (2010) Diclofenac: an update on its mechanism of action and safety profile. Curr Med Res Opin 26(7):1715–1731. https://doi.org/10.1185/03007995.2010.486301
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interests or disclosures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Loh, J.W., Taib, N.A., Cheong, Y.T. et al. A Double-Blind, Randomized Controlled Trial of Pre-incision Wound Infiltration Using Diclofenac Versus Bupivacaine for Post-operative Pain Relief in Open Thyroid and Parathyroid Surgery. World J Surg 44, 2656–2666 (2020). https://doi.org/10.1007/s00268-020-05458-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05458-6