Abstract
Introduction
Secondary overtriage (OT) is the unnecessary transfer of injured patients between facilities. In low- and middle-income countries (LMICs), which shoulder the greatest burden of trauma globally, the impact of wasted resources on an overburdened system is high. This study determined the rate and associated characteristics of OT at a Malawian central hospital.
Methods
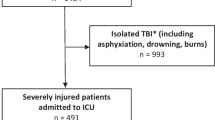
A retrospective analysis of prospectively collected data from January 2012 through July 2017 was performed at Kamuzu Central Hospital (KCH) in Lilongwe, Malawi. Patients were considered OT if they were discharged alive within 48 h without undergoing a procedure, and were not severely injured or in shock on arrival. Factors evaluated for association with OT included patient demographics, injury characteristics, and transferring facility information.
Results
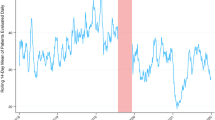
Of 80,915 KCH trauma patients, 15,422 (19.1%) transferred from another facility. Of these, 8703 (56.2%) were OT. OT patients were younger (median 15, IQR: 6–31 versus median 26, IQR: 11–38, p < 0.001). Patients with primary extremity injury (5308, 59.9%) were overtriaged more than those with head injury (1991, 51.8%) or torso trauma (1349, 50.8%), p < 0.001. The OT rate was lower at night (18.9% v 28.7%, p < 0.001) and similar on weekends (20.4% v 21.8%, p = 0.03). OT was highest for penetrating wounds, bites, and falls; burns were the lowest. In multivariable modeling, risk of OT was greatest for burns and soft tissue injuries.
Conclusions
The majority of trauma patients who transfer to KCH are overtriaged. Implementation of transfer criteria, trauma protocols, and interhospital communication can mitigate the strain of OT in resource-limited settings.

Similar content being viewed by others
References
Mock C, Joshipura M, Arreola-Risa C et al (2012) An estimate of the number of lives that could be saved through improvements in trauma care globally. World J Surg 36:959–963. https://doi.org/10.1007/s00268-012-1459-6
Reynolds TA, Stewart B, Drewett I et al (2017) The impact of trauma care systems in low- and middle-income countries. Annu Rev Public Health 38:507–532
Aaronson E, Mort E, Soghoian S (2017) Mapping the process of emergency care at a teaching hospital in Ghana. Healthc (Amst) 5:214–220
Kubwimana O (2018) Elaborated plan for incoming surgical emergency management in Sub-Saharan Africa. Open Access Emerg Med 10:67–70
Harmsen AM, Giannakopoulos GF, Moerbeek PR et al (2015) The influence of prehospital time on trauma patients outcome: a systematic review. Injury 46:602–609
Tang A, Hashmi A, Pandit V et al (2014) A critical analysis of secondary overtriage to a Level I trauma center. J Trauma Acute Care Surg 77:969–973
Ciesla DJ, Sava JA, Street JH 3rd et al (2008) Secondary overtriage: a consequence of an immature trauma system. J Am Coll Surg 206:131–137
Con J, Long D, Sasala E et al (2015) Secondary overtriage in a statewide rural trauma system. J Surg Res 198:462–467
Sorensen MJ, von Recklinghausen FM, Fulton G et al (2013) Secondary overtriage: the burden of unnecessary interfacility transfers in a rural trauma system. JAMA Surg 148:763–768
Abebe Y, Dida T, Yisma E et al (2018) Ambulance use is not associated with patient acuity after road traffic collisions: a cross-sectional study from Addis Ababa, Ethiopia. BMC Emerg Med 18:7
Cannon CM, Braxton CC, Kling-Smith M et al (2009) Utility of the shock index in predicting mortality in traumatically injured patients. J Trauma 67:1426–1430
Gallaher J, Jefferson M, Varela C et al (2019) The Malawi trauma score: a model for predicting trauma-associated mortality in a resource-poor setting. Injury 50:1552–1557
Eastwood K, Smith K, Morgans A et al (2017) Appropriateness of cases presenting in the emergency department following ambulance service secondary telephone triage: a retrospective cohort study. BMJ Open 7:e016845
Famoye F, Rothe DE (2003) Variable selection for Poisson regression model. J Mod Appl Stat Methods 2:11
Knol MJ, Le Cessie S, Algra A et al (2012) Overestimation of risk ratios by odds ratios in trials and cohort studies: alternatives to logistic regression. CMAJ 184:895–899
Mbengue MAS, Chasela C, Onoya D et al (2019) Clinical predictor score to identify patients at risk of poor viral load suppression at six months on antiretroviral therapy: results from a prospective cohort study in Johannesburg, South Africa. Clin Epidemiol 11:359–373
Zou G (2004) A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 159:702–706
Laytin AD, Kumar V, Juillard CJ et al (2015) Choice of injury scoring system in low- and middle-income countries: lessons from Mumbai. Injury 46:2491–2497
Kawooya MG (2012) Training for rural radiology and imaging in sub-saharan Africa: addressing the mismatch between services and population. J Clin Imaging Sci 2:37
Littman-Quinn R, Mibenge C, Antwi C et al (2013) Implementation of m-health applications in Botswana: telemedicine and education on mobile devices in a low resource setting. J Telemed Telecare 19:120–125
Bracale M, Pepino A (1994) Medical technologies in developing countries: a feasibility study on the maintenance of medical equipment in Ethiopia. Med Biol Eng Comput 32:131–137
Gajewski J, Bijlmakers L, Mwapasa G et al (2018) ‘I think we are going to leave these cases’. Obstacles to surgery in rural Malawi: a qualitative study of provider perspectives. Trop Med Int Health 23:1141–1147
Gajewski J, Pittalis C, Lavy C, et al (2019) Anesthesia capacity of district-level hospitals in Malawi, Tanzania, and Zambia: a mixed-methods study. Anesth Analg. https://doi.org/10.1213/ANE.0000000000004363
van Amelsfoort JJ, van Leeuwen PA, Jiskoot P et al (2010) Surgery in Malawi—the training of clinical officers. Trop Dr 40:74–76
Bastawrous A, Armstrong MJ (2013) Mobile health use in low-and high-income countries: an overview of the peer-reviewed literature. J R Soc Med 106:130–142
Kim J, Barreix M, Babcock C et al (2017) Acute care referral systems in Liberia: transfer and referral capabilities in a low-income country. Prehosp Disaster Med 32:642–650
Augestad KM, Bellika JG, Budrionis A et al (2013) Surgical telementoring in knowledge translation—clinical outcomes and educational benefits: a comprehensive review. Surg Innov 20:273–281
Augestad KM, Han H, Paige J et al (2017) Educational implications for surgical telementoring: a current review with recommendations for future practice, policy, and research. Surg Endosc 31:3836–3846
Erridge S, Yeung DKT, Patel HRH et al (2018) Telementoring of surgeons: a systematic review. Surg Innov 26:95–111
Pittalis C, Brugha R, Crispino G et al (2019) Evaluation of a surgical supervision model in three African countries—protocol for a prospective mixed-methods controlled pilot trial. Pilot Feasibility Stud 5:25
Funding
This research did not receive external Grant funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflict to declare.
Ethical approval
This study was approved by both University of North Carolina IRB and the Malawian National Health Science Research Council, who waved the need for individual consent given the nature of the study design.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Maine, R.G., Kajombo, C., Mulima, G. et al. Secondary Overtriage of Trauma Patients to a Central Hospital in Malawi. World J Surg 44, 1727–1735 (2020). https://doi.org/10.1007/s00268-020-05426-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05426-0