Abstract
Objectives
To evaluate enhanced recovery after surgery (ERAS) protocols in emergency abdominal surgery.
Methods
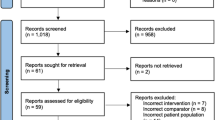
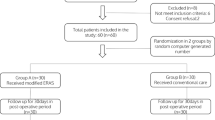
The electronic data sources were explored to capture all studies that evaluated the impact of ERAS protocols in patients who underwent emergency abdominal surgery. The quality of randomised and non-randomised studies was evaluated by the Cochrane tool and the Newcastle–Ottawa scale, respectively. Random or fixed effects modelling were utilised as indicated.
Results
Six comparative studies, enrolling 1334 patients, were eligible. ERAS protocols resulted in shorter post-operative time to first flatus (mean difference: −1.40, P < 0.00001), time to first defecation (mean difference: −1.21, P = 0.02), time to first oral liquid diet (mean difference: −2.30, P < 0.00001), time to first oral solid diet (mean difference: −2.40, P < 0.00001) and length of hospital stay (mean difference: −3.09, −2.80, P < 0.00001). ERAS protocols also resulted in lower risks of total complications (odds ratio: 0.50, P < 0.00001), major complications (odds ratio: 0.60, P = 0.0008), pulmonary complications (odds ratio: 0.38, P = 0.0003), paralytic ileus (odds ratio: 0.53, 0.88, P = 0.01) and surgical site infection (odds ratio: 0.39, P = 0.0001). Both ERAS and non-ERAS protocols resulted in similar risk of 30-day mortality (risk difference: −0.00, P = 0.94), need for re-admission (risk difference: −0.01, P = 0.50) and need for re-operation (odds ratio: 0.83, P = 0.50).
Conclusions
Although ERAS protocols are commonly used in elective settings, they are associated with favourable outcomes in emergency settings as indicated by reduced post-operative complications, accelerated recovery of bowel function and shorter post-operative hospital stay without increasing need for re-admission or re-operation. There should be an effort to incorporate ERAS protocols into emergency abdominal surgery settings.





Similar content being viewed by others
References
Fearon KC, Ljungqvist O, Von Meyenfeldt M, Revhaug A, Dejong CH, Lassen K et al (2005) Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr 24(3):466–477
Watt DG, McSorley ST, Horgan PG, McMillan DC (2015) Enhanced recovery after surgery: which components, if any, impact on the systemic inflammatory response following colorectal surgery? A systematic review. Medicine (Baltimore) 94(36):e1286
Basse L, Raskov HH, Hjort Jakobsen D, Sonne E, Billesbølle P, Hendel HW et al (2002) Accelerated postoperative recovery programme after colonic resection improves physical performance, pulmonary function and body composition. Br J Surg 89:446–453
Barbieri A, Vanhaecht K, Van Herck P, Sermeus W, Faggiano F, Marchisio S et al (2009) Effects of clinical pathways in the joint replacement: a meta-analysis. BMC Med 7:32
Azhar RA, Bochner B, Catto J, Goh AC, Kelly J, Patel HD et al (2016) Enhanced recovery after urological surgery: a contemporary systematic review of outcomes, key elements, and research needs. Eur Urol 70:176–187
Arsalani-Zadeh R, ElFadl D, Yassin N, MacFie J (2011) Evidence-based review of enhancing postoperative recovery after breast surgery. Br J Surg 98:181–196
Hughes MJ, McNally S, Wigmore SJ (2014) Enhanced recovery following liver surgery: a systematic review and meta-analysis. HPB (Oxford) 16:699–706
Pisarska M, Małczak P, Major P, Wysocki M, Budzyński A, Pędziwiatr M (2017) Enhanced recovery after surgery protocol in oesophageal cancer surgery: systematic review and meta-analysis. PLoS ONE 12:e0174382
de Groot JJ, Ament SM, Maessen JM, Dejong CH, Kleijnen JM, Slangen BF (2016) Enhanced recovery pathways in abdominal gynecologic surgery: a systematic review and meta-analysis. Acta Obstet Gynecol Scand 95:382–395
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Lassen K, Soop M, Nygren J, Cox PB, Hendry PO, Spies C et al (2009) Consensus review of optimal perioperative care in colorectal surgery: enhanced Recovery After Surgery (ERAS) Group recommendations. Arch Surg 144:961–969
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/nos_manual.pdf. Accessed 19 Apr 2019
Shang Y, Guo C, Zhang D (2018) Modified enhanced recovery after surgery protocols are beneficial for postoperative recovery for patients undergoing emergency surgery for obstructive colorectal cancer: a propensity score matching analysis. Medicine (Baltimore) 97(39):e12348
Mohsina S, Shanmugam D, Sureshkumar S, Kundra P, Mahalakshmy T, Kate V (2018) Adapted ERAS pathway vs. standard care in patients with perforated duodenal ulcer—a randomized controlled trial. J Gastrointest Surg. J 22(1):107–116
Shida D, Tagawa K, Inada K, Nasu K, Seyama Y, Maeshiro T et al (2017) Modified enhanced recovery after surgery (ERAS) protocols for patients with obstructive colorectal cancer. BMC Surg 17(1):18
Wisely JC, Barclay KL (2016) Effects of an Enhanced Recovery After Surgery programme on emergency surgical patients. ANZ J Surg 86(11):883–888
Gonenc M, Dural AC, Celik F, Akarsu C, Kocatas A, Kalayci MU et al (2014) Enhanced postoperative recovery pathways in emergency surgery: a randomised controlled clinical trial. Am J Surg 207(6):807–814
Lohsiriwat V (2014) Enhanced recovery after surgery vs conventional care in emergency colorectal surgery. World J Gastroenterol 20(38):13950–13955
Ji HB, Zhu WT, Wei Q, Wang XX, Wang HB, Chen QP (2018) Impact of enhanced recovery after surgery programs on pancreatic surgery: a meta-analysis. World J Gastroenterol 24(15):1666–1678
Wang LH, Zhu RF, Gao C, Wang SL, Shen LZ (2018) Application of enhanced recovery after gastric cancer surgery: an updated meta-analysis. World J Gastroenterol 24(14):1562–1578
Li L, Chen J, Liu Z, Li Q, Shi Y (2017) Enhanced recovery program versus traditional care after hepatectomy: a meta-analysis. Medicine (Baltimore) 96(38):e8052
Pisarska M, Małczak P, Major P, Wysocki M, Budzyński A, Pędziwiatr M (2017) Enhanced recovery after surgery protocol in oesophageal cancer surgery: systematic review and meta-analysis. PLoS ONE 12(3):e0174382
Spanjersberg WR, van Sambeeck JD, Bremers A, Rosman C, van Laarhoven CJ (2015) Systematic review and meta-analysis for laparoscopic versus open colon surgery with or without an ERAS programme. Surg Endosc 29(12):3443–3453
Shuldham C (1999) A review of the impact of pre-operative education on recovery from surgery. Int J Nurs Stud 36:171–177
Sethi A, Debbarma M, Narang N, Saxena A, Mahobia M, Tomar GS (2018) Impact of targeted preoperative optimization on clinical outcome in emergency abdominal surgeries: a prospective randomized trial. Anesth Essays Res 12:149–154
Bilgin H (2017) Inadverdent perioperative hypothermia. Turk J Anaesthesiol Reanim 45:124–126
Huddart S, Peden CJ, Swart M, McCormick B, Dickinson M, Mohammed MA et al (2015) Use of a pathway quality improvement care bundle to reduce mortality after emergency laparotomy. Br J Surg 102:57–66
Sapkota R, Bhandari RS (2013) Prophylactic nasogastric decompression after emergency laparotomy. JNMA J Nepal Med Assoc 52:437–442
Lohsiriwat V (2016) Pelvic drain after colorectal anastomosis: useful or useless. Transl Cancer Res 5:S1404–S1407
Klappenbach RF, Yazyi FJ, Alonso Quintas F, Horna ME, Alvarez Rodríguez J, Oría A (2013) Early oral feeding versus traditional postoperative care after abdominal emergency surgery: a randomized controlled trial. World J Surg 37:2293–2299. https://doi.org/10.1007/s00268-013-2143-1
Boden I, Sullivan K, Hackett C, Winzer B, Lane R, McKinnon M et al (2018) ICEAGE (Incidence of Complications following Emergency Abdominal surgery: Get Exercising): study protocol of a pragmatic, multicentre, randomised controlled trial testing physiotherapy for the prevention of complications and improved physical recovery after emergency abdominal surgery. World J Emerg Surg 13:29
Funding
There were no funding resources for this study
Author information
Authors and Affiliations
Contributions
SH was the lead of the project and designed the study. SH and SH performed the statistical analyses required in this study and wrote the first draft of the article. All authors contributed to collection of data, revision of the first draft and approving the final version of the article
Corresponding author
Ethics declarations
Conflict of interest
All authors confirmed that they had no conflict of interest.
Ethical approval
Ethical approval was not required for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Search | Search description | |
|---|---|---|
Search #1 | enhance* near2 recovery | T, A, K |
Search #2 | ERAS | T, A, K |
Search #3 | Search #1 OR Search #2 | Combined with OR |
Search #4 | emergency near2 surgery | T, A, K |
Search #5 | MeSH term: [laparotomy] | explode all trees |
Search #6 | emergency near2 laparotomy | T, A, K |
Search #7 | Search #4 OR Search #5 OR Search #6 | Combined with OR |
Search #8 | Search #3 AND Search #7 | Combined with AND |
Rights and permissions
About this article
Cite this article
Hajibandeh, S., Hajibandeh, S., Bill, V. et al. Meta-analysis of Enhanced Recovery After Surgery (ERAS) Protocols in Emergency Abdominal Surgery. World J Surg 44, 1336–1348 (2020). https://doi.org/10.1007/s00268-019-05357-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-05357-5