Abstract
Objective
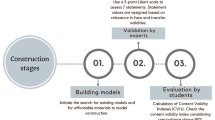
To assess the content validity of a low-cost bench-top model (“Raj Model”) for the training of laparoscopic port insertion at the Urology Simulation Bootcamp course (USBC).
Materials and methods
A low-cost abdominal wall model of 40 × 40 cm was created to simulate laparoscopic port placement. The model was made using different synthetic materials to represent layers (skin—vinyl sheet, subcutaneous fat—10 mm soft foam, anterior rectus sheath and muscle—floor mat, posterior rectus sheath—masking wall tape, peritoneum—sellotape). Each model was used by up to 3 trainees to practise laparoscopic port placement. The model was assessed for content validity by trainees and experts using a 5-point Likert scale.
Result
In total, 88 trainees and 6 experts participated in the study. For all aspects of the synthetic abdominal wall, good (4) or very good (5) scores ranged from 52.7–69.2%, whereas very poor (1) rating ranged from 0 to 4.3%. There was no significant difference in responses for the content validity of the model between trainees and experts. There was a high intraclass correlation amongst responses from trainees (0.89) and experts (0.79). Approximately 76.3% of trainees and experts felt that the model is suitable for training.
Conclusion
This is the first validation study of a low-cost abdominal wall model for teaching laparoscopic port placement for trainees. Our study demonstrates that this synthetic model has high content validity and is useful for surgical training.


Similar content being viewed by others
Abbreviations
- USBC:
-
Urology simulation bootcamp course
- EWTR:
-
European working time regulations
- JCST:
-
Joint committee on surgical training
- VR:
-
Virtual reality
References
Giles JA (2010) Surgical training and the European working time directive: the role of informal workplace learning. Int J Surg 8(3):179–180
England RCoSo (2015) Improving surgical training: proposal for pilot surgical training programme, pp 12–13
Flanders D, Pirpiris A, Corcoran N, Forsyth R, Grills R (2019) Lessons learned and new challenges: re-evaluation of end-user assessment of a skills-based training program for urology trainees. J Med Educ Curric Dev 6:2382120519834552
Pena G, Altree M, Field J, Sainsbury D, Babidge W, Hewett P et al (2015) Nontechnical skills training for the operating room: a prospective study using simulation and didactic workshop. Surgery 158(1):300–309
Brewin J, Ahmed K, Khan MS, Jaye P, Dasgupta P (2014) Face, content, and construct validation of the Bristol TURP trainer. J Surg Educ 71(4):500–505
Sutherland LM, Middleton PF, Anthony A, Hamdorf J, Cregan P, Scott D et al (2006) Surgical simulation: a systematic review. Ann Surg 243(3):291–300
Young M, Kailavasan M, Taylor J, Cornford P, Colquhoun A, Rochester M et al (2019) The success and evolution of a urological “Boot Camp” for newly appointed UK urology registrars: incorporating simulation, nontechnical skills and assessment. J Surg Educ 76(5):1425–1432
JCoST (JCST) (2018) Quality indicators for surgical training: core surgical training (2018). https://www.jcst.org/-/media/files/jcst/quality-assurance/quality-indicators/core-qis–final-v8.pdf. Accessed July 2019
Tan SC, Marlow N, Field J, Altree M, Babidge W, Hewett P et al (2012) A randomized crossover trial examining low- versus high-fidelity simulation in basic laparoscopic skills training. Surg Endosc 26(11):3207–3214
Steigerwald SN, Park J, Hardy KM, Gillman LM, Vergis AS (2015) Does laparoscopic simulation predict intraoperative performance? A comparison between the fundamentals of laparoscopic surgery and LapVR evaluation metrics. Am J Surg 209(1):34–39
Schout BM, Hendrikx AJ, Scheele F, Bemelmans BL, Scherpbier AJ (2010) Validation and implementation of surgical simulators: a critical review of present, past, and future. Surg Endosc 24(3):536–546
Acknowledgements
We are grateful to all laparoscopic module faculty members (Mr N Vasdev, Mr N Eroneni, Mr G Lewis, Mr S Pathak, Mr R Rajasundaram, Mr J Levickis, Mr R Veerattarapillay) and Leeds Medical Education staff for their fantastic support.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Study concept and design: CSB, BG; Acquisition of data: MK, CB, GK, BR, BW, SJ; Analysis and interpretation: MK, CB; Study supervision: CSB, BG.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kailavasan, M., Berridge, C., Kandaswamy, G. et al. A Low-Cost Synthetic Abdominal Wall Model (“Raj Model”) for the Training of Laparoscopic Port Insertion. World J Surg 44, 1431–1435 (2020). https://doi.org/10.1007/s00268-019-05354-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-05354-8