Abstract
Background
Multidrug-resistant (MDR) bacteria are an emerging international concern in low- and middle-income countries that threaten recent public health gains. These challenges are exacerbated in immunocompromised hosts, such as those with burn injury. This study sought to describe the epidemiology and associated clinical outcomes of burn wound colonization in a Malawian tertiary burn center.
Methods
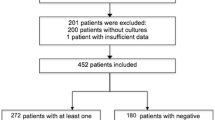
This is a prospective analysis of burn patients presenting to Kamuzu Central Hospital in Lilongwe, Malawi, within 72 h of burn injury. A swab of each patient’s primary wound was collected at admission and each subsequent week. The primary exposure was burn wound colonization with MDR bacteria, particularly Enterobacteriaceae. The primary outcome was in-hospital mortality. A log binomial model estimated the association between the exposure and outcome, adjusted for confounders.
Results
Ninety-nine patients were enrolled with a median age of 4 years (IQR 2–12) and a male preponderance (54%). Median total body surface area burn (TBSA) was 14% (IQR 9–25), and crude in-hospital mortality was 19%. Enterobacteriaceae were the most common MDR bacteria with 36% of patients becoming colonized. Wound colonization with MDR Enterobacteriaceae was associated with increased in-hospital mortality with a risk ratio of 1.86 (95% CI 1.38, 2.50, p < 0.001) adjusted for TBSA, burn type (scald vs. flame), sex, age, length of stay, and methicillin-resistant Staphylococcus aureus colonization.
Conclusion
MDR bacteria, especially Enterobacteriaceae, are common and are associated with worse burn injury outcomes. In resource-poor environments, a greater emphasis on prevention of MDR bacterial colonization, improved isolation precautions, affordable diagnostics, and antibiotic stewardship are imperative.

Similar content being viewed by others
Data availability
Jared R. Gallaher, MD, MPH and Anthony G. Charles, MD, MPH had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
References
Tseng SH, Lee CM, Lin TY et al (2011) Emergence and spread of multi-drug resistant organisms: think globally and act locally. J Microbiol Immunol Infect 44(3):157–165
Spellberg B, Guidos R, Gilbert D et al (2008) The epidemic of antibiotic-resistant infections: a call to action for the medical community from the Infectious Diseases Society of America. Clin Infect Dis 46(2):155–164
World Health Organization (2014) Antimicrobial resistance: 2014 global report on surveillance. http://apps.who.int/iris/bitstream/10665/112642/1/9789241564748_eng.pdf. Accessed 08 May 2017
Zhang R, Eggleston K, Rotimi V et al (2006) Antibiotic resistance as a global threat: evidence from China, Kuwait and the United States. Glob Health 2(1):6
Okeke IN (2006) Diagnostic insufficiency in Africa. Clin Infect Dis 42:1501–1503
Petti CA, Polage CR, Quinn TC et al (2006) Laboratory medicine in Africa: a barrier to effective health care. Clin Infect Dis 42:377–382
World Health Organization (2015) Global action plan on antimicrobial resistance. http://www.who.int/antimicrobial-resistance/publications/global-action-plan/en/. Accessed 08 May 2017
Falagas ME, Karageorgopoulos DE (2008) Pandrug resistance (PDR), extensive drug resistance (XDR), and multidrug resistance (MDR) among gram-negative bacilli: need for international harmonization in terminology. Clin Infect Dis 46(7):1121–1122
World Health Organization (2004) The Global Burden of Disease: 2004 update. http://www.wo.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf. Accessed 08 May 2017
Mayhall CG (2003) The epidemiology of burn wound infections: then and now. Clin Infect Dis 37:543–550
Boucher HW, Talbot GH, Bradley JS et al (2009) Bad bugs, no drugs: no ESKAPE! An update from the infectious diseases Society of America. Clin Infect Dis 48:1–12
Kanamori H, Parobek CM, Juliano JJ et al (2017) A prolonged outbreak of KPC-3-producing Enterobacter cloacae and Klebsiella pneumoniae driven by multiple mechanisms of resistance transmission at a large academic burn center. Antimicrob Agents Chemother 61(2):e01516
Samuel JC, Campbell EL, Mjuweni S et al (2011) The epidemiology, management, outcomes and areas for improvement of burn care in central Malawi: an observational study. J Int Med Res 39(3):873–879
Magiorakos AP, Srinivasan A, Carey RB et al (2012) Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 18:268–281
CLSI Clinical and Laboratory Standards Institute (2006) Performance standards for antimicrobial susceptibility testing Sixteenth informational supplement. Clinical and Laboratory Standards Institute, Chicago (Document M100-S16)
Tyson AF, Boschini LP, Kiser MM et al (2013) Survival after burn in a sub-Saharan burn unit: challenges and opportunities. Burns 39(8):1619–1625
Gallaher JR, Mjuweni S, Shah M et al (2015) Timing of early excision and grafting following burn injury in Sub-Saharan Africa. Burns 41(6):1353–1359
Burroughs T, Najafi M, Lemon SM et al (2003) The resistance phenomenon in microbes and infectious disease vectors: implications for human health and strategies for containment–workshop summary. National Academies Press, Washington
Sosa AD, Amábile-Cuevas CF, Byarugaba DK et al (2010) Antimicrobial resistance in developing countries. Springer, New York
Petti CA, Polage CR, Quinn TC et al (2006) Laboratory medicine in Africa: a barrier to effective health care. Clin Infect Dis 42(3):377–382
Fadeyibi IO, Raji MA, Ibrahim NA et al (2013) Bacteriology of infected burn wounds in the burn wards of a teaching hospital in Southwest Nigeria. Burns 39(1):168–173
Komolafe OO, James J, Kalongolera L et al (2003) Bacteriology of burns at the Queen Elizabeth Central Hospital, Blantyre, Malawi. Burns 29(3):235–238
Livimbi OM, Komolafe IO (2007) Epidemiology and bacterial colonization of burn injuries in Blantyre, Malawi. Med J 19(1):25–27
Amissah NA, van Dam L, Ablordey A et al (2017) Epidemiology of Staphylococcus aureus in a burn unit of a tertiary care center in Ghana. PLoS ONE 12(7):e0181072
Essayagh M, Essayagh T, Essayagh S et al (2014) Epidemiology of burn wound infection in Rabat, Morocco: three-year review. Med Sante Trop 24(2):157–164
Elmanama AA, Al Laham NA, Tayh GA (2013) Antimicrobial susceptibility of bacterial isolates from burn units in Gaza. Burns 39(8):1612–1618
Ahmad M, Hussain SS, Khan MI et al (2006) Pattern of bacterial invasion in burn patients at the Pakistan Institute of Medical Sciences, Islamabad. Ann Burns Fire Disasters 19(1):18
Nasser S, Mabrouk A, Maher A (2003) Colonization of burn wounds in Ain Shams University burn unit. Burns 29(3):229–233
Perwee N, Prakash SK, Siddiqui O (2015) Multi drug resistant Klebsiella isolates in burn patients: a comparative study. JCDR 9(9):14
Ronat JB, Kakol J, Khoury MN et al (2014) Highly drug-resistant pathogens implicated in burn-associated bacteremia in an Iraqi burn care unit. PLoS ONE 9(8):e101017
Erol S, Altoparlak U, Akcay MN (2004) Changes of microbial flora and wound colonization in burned patients. Burns 30(4):357–361
Singh NP, Goyal R, Manchanda V (2003) Changing trends in bacteriology of burns in the burns unit, Delhi, India. Burns 29(2):129–132
Hassuna NA, Mohamed AH, Abo-Eleuoon SM, et al (2015) High prevalence of multidrug resistant Pseudomonas aeruginosa recovered from infected burn wounds in children. Arch Clin Microbiol 6(4):1
van Langeveld I, Gagnon RC, Conrad PF et al (2017) Multiple-drug resistance in burn patients: a retrospective study on the impact of antibiotic resistance on survival and length of stay. J Burn Care Res 38(2):99–105
Theodorou P, Thamm OC, Perbix W et al (2013) Pseudomonas aeruginosa bacteremia after burn injury: the impact of multiple-drug resistance. J Burn Care Res 34(6):649–658
Raz-Pasteur A, Fishel R, Hardak E et al (2016) Do wound cultures give information about the microbiology of blood cultures in severe burn patients? Ann Plast Surg 76(1):34–39
Gang RK, Sanyal SC, Bang RL et al (2000) Staphylococcal septicaemia in burns. Burns 26(4):359–366
Chong SJ, Ahmed S, Tay JM (2011) 5 year analysis of bacteriology culture in a tropical burns ICU. Burns 37(8):1349–1353
Barret JP, Herndon DN (2003) Effects of burn wound excision on bacterial colonization and invasion. Plast Reconstr Surg 111(2):744–750
Subcommittee S, Subcommittee A, ISBI Practice Guidelines Committee (2016) ISBI practice guidelines for burn care. Burns 42(5):953–1021
World Health Organization (2017) WHO publishes list of bacteria for which new antibiotics are urgently needed. http://www.who.int/mediacentre/news/releases/2017/bacteria-antibiotics-needed/en. Accessed 08 May 2017
Church D, Elsayed S, Reid O, Winston B, Lindsay R (2006) Burn wound infections. Clin Microbiol Rev 19(2):403–434
Funding
Funding was provided by the North Carolina Jaycee Burn Center in the Department of Surgery at the University of North Carolina and a grant from the UNC Womack Surgical Society. A.M.L is supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant KL2TR001109. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
JRG, MD, MPH contributed to this paper by design of study, acquisition, analysis, and interpretation of data, drafting and revision of the manuscript, and statistical analysis. AML, MD, MPH contributed to this paper by interpretation of data, critical drafting and revision of the manuscript, and statistical analysis. WB, MB, BS contributed to this paper by design of study, critical revision of the manuscript for important intellectual content, and administrative and technical support. RK, MS contributed to this paper by design of study, acquisition of data, critical revision of the manuscript for important intellectual content, and administrative and technical support. BAC, MD contributed to this paper by design of the study, revision of the manuscript for important intellectual content, supervision, and the obtaining of funding. AGC, MD, MPH contributed to this paper by conception and design of the study, acquisition, analysis, and interpretation of data, drafting and revision of the manuscript, statistical analysis, obtaining of funding, and supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to disclose. The authors have no financial relationships to disclose. A.M.L.: Destum Partners and KPB Biosciences, Consulting. GlaxoSmithKline, Research funding. No other disclosures.
Rights and permissions
About this article
Cite this article
Gallaher, J.R., Banda, W., Lachiewicz, A.M. et al. Colonization with Multidrug-Resistant Enterobacteriaceae is Associated with Increased Mortality Following Burn Injury in Sub-Saharan Africa. World J Surg 42, 3089–3096 (2018). https://doi.org/10.1007/s00268-018-4633-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4633-7