Abstract
Objective
Albumin–bilirubin (ALBI) grade has been validated as a simple, evidence-based, and objective prognostic tool for patients with hepatocellular carcinoma (HCC). However, minimal information is available concerning postoperative ALBI grade changes in HCC. This study aimed to investigate the prognostic value of postoperative ALBI grade changes in patients with hepatitis B virus (HBV)-related HCC within the Milan criteria after liver resection.
Methods
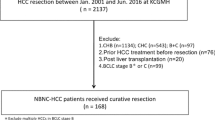
Patients with HBV-related HCC within the Milan criteria who underwent liver resection between 2010 and 2016 at West China Hospital were reviewed (N = 258). A change in ALBI grade was defined as first postoperative month ALBI grade–preoperative ALBI grade. If the value was >0, postoperative worsening of ALBI grade was considered; otherwise, stable ALBI grade was considered. Cox proportional hazard regression analyses were used to determine the factors that influence recurrence and survival.
Results
During the follow-up, 130 patients experienced recurrence and 47 patients died. Multivariate analyses revealed that postoperative worsening of ALBI grade (HR 1.541, 95% CI 1.025–2.318, P = 0.038), microvascular invasion (MVI, HR 1.802, 95% CI 1.205–2.695, P = 0.004), and multiple tumors (HR 1.676, 95% CI 1.075–2.615, P = 0.023) were associated with postoperative recurrence, whereas MVI (HR 2.737, 95% CI 1.475–5.080, P = 0.001), postoperative worsening of ALBI grade (HR 2.268, 95% CI 1.227–4.189, P = 0.009), high alpha-fetoprotein level (HR 2.055, 95% CI 1.136–3.716, P = 0.017), and transfusion (HR 2.597, 95% CI 1.395–4.834, P = 0.003) negatively influenced long-term survival. Patients with postoperative worsening of ALBI grade exhibited increased incidence of recurrence and worse long-term survival.
Conclusion
Postoperative worsening of ALBI grade was associated with increased recurrence and poorer overall survival for patients with HBV-related HCC within the Milan criteria. We should pay attention to liver function changes in HCC patients after liver resection.

Similar content being viewed by others
Abbreviations
- AFP:
-
Alpha-fetoprotein
- ALBI:
-
Albumin–bilirubin grade
- HBV:
-
Hepatitis B virus
- HCC:
-
Hepatocellular carcinoma
- MVI:
-
Microvascular invasion
- NLR:
-
Neutrophil to lymphocyte rate
- OS:
-
Overall survival
- RFS:
-
Recurrence-free survival
- TNM:
-
Tumor-node-metastasis
References
Cabre N, Camps J, Joven J (2016) Inflammation, mitochondrial metabolism and nutrition: the multi-faceted progression of non-alcoholic fatty liver disease to hepatocellular carcinoma. Hepatobiliary Surg Nutr 5:438–443
Torre LA, Bray F, Siegel RL et al (2015) Global cancer statistics, 2012. CA Cancer J Clin 65:87–108
Parkin DM, Bray F, Ferlay J et al (2005) Global cancer statistics, 2002. CA Cancer J Clin 55:74–108
Poon RT, Fan ST, Lo CM et al (2002) Long-term survival and pattern of recurrence after resection of small hepatocellular carcinoma in patients with preserved liver function: implications for a strategy of salvage transplantation. Ann Surg 235(373–38):2
Johnson PJ, Berhane S, Kagebayashi C et al (2015) Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol 33(550–55):8
Gui B, Weiner AA, Nosher J et al (2017) Assessment of the albumin–bilirubin (ALBI) grade as a prognostic indicator for hepatocellular carcinoma patients treated with radioembolization. Am J Clin Oncol. https://doi.org/10.1097/COC.0000000000000384
Wang YY, Zhong JH, Su ZY et al (2016) Albumin–bilirubin versus Child–Pugh score as a predictor of outcome after liver resection for hepatocellular carcinoma. Br J Surg 103(725–73):4
Toyoda H, Lai PB, O’Beirne J et al (2016) Long-term impact of liver function on curative therapy for hepatocellular carcinoma: application of the ALBI grade. Br J Cancer 114:744–775
Li C, Zhu WJ, Wen TF et al (2014) Child–Pugh A hepatitis B-related cirrhotic patients with a single hepatocellular carcinoma up to 5 cm: liver transplantation vs. resection. J Gastrointest Surg 18:1469–1476
Kubo H, Murayama Y, Arita T et al (2016) The prognostic value of preoperative neutrophil-to-lymphocyte ratio in colorectal cancer. World J Surg 40(2796–280):2. https://doi.org/10.1007/s00268-016-3595-x
Yang SL, Liu LP, Yang S et al (2016) Preoperative serum alpha-fetoprotein and prognosis after hepatectomy for hepatocellular carcinoma. Br J Surg 103(716–72):4
Kauffmann R, Fong Y (2014) Post-hepatectomy liver failure. Hepatobiliary Surg Nutr 3(238–24):6
Hallet J, Karanicolas PJ, Zih FS et al (2016) Hypophosphatemia and recovery of post-hepatectomy liver insufficiency. Hepatobiliary Surg Nutr 5(217–22):4
Wrighton LJ, O’Bosky KR, Namm JP et al (2012) Postoperative management after hepatic resection. J Gastrointest Oncol 3(41–4):7
Zhao H, Chen C, Gu S et al (2017) Anatomical versus non-anatomical resection for solitary hepatocellular carcinoma without macroscopic vascular invasion: a propensity score matching analysis. J Gastroenterol Hepatol 32(870–87):8
Schlichtemeier SM, Pang TC, Williams NE et al (2016) A pre-operative clinical model to predict microvascular invasion and long-term outcome after resection of hepatocellular cancer: The Australian experience. Eur J Surg Oncol 42(1576–158):3
Lei Z, Li J, Wu D et al (2016) Nomogram for preoperative estimation of microvascular invasion risk in hepatitis B virus-related hepatocellular carcinoma within the Milan criteria. JAMA Surg 151(356–36):3
Grazi GL, Cescon M, Ravaioli M et al (2003) Liver resection for hepatocellular carcinoma in cirrhotics and noncirrhotics. Evaluation of clinicopathologic features and comparison of risk factors for long-term survival and tumour recurrence in a single centre. Aliment Pharmacol Ther 17(Suppl 2):119–129
Iguchi K, Hatano E, Yamanaka K et al (2014) The impact of posthepatectomy liver failure on the recurrence of hepatocellular carcinoma. World J Surg 38(150–15):8. https://doi.org/10.1007/s00268-013-2247-7
Fukushima K, Fukumoto T, Kuramitsu K et al (2014) Assessment of ISGLS definition of posthepatectomy liver failure and its effect on outcome in patients with hepatocellular carcinoma. J Gastrointest Surg 18(729–73):6
Nachnani JS, Hamid F, Pandya P et al (2010) Transfusion-related acute hepatic enzyme elevation: a new disease entity? Eur J Gastroenterol Hepatol 22:378
Sahu S, Hemlata AV (2014) Adverse events related to blood transfusion. Indian J Anaesth 58:543–551
Motoyama H, Kobayashi A, Yokoyama T et al (2014) Liver failure after hepatocellular carcinoma surgery. Langenbecks Arch Surg 399(1047–105):5
Sima CS, Jarnagin WR, Fong Y et al (2009) Predicting the risk of perioperative transfusion for patients undergoing elective hepatectomy. Ann Surg 250(914–92):1
Bagante F, Spolverato G, Ruzzenente A et al (2016) Validation of a nomogram to predict the risk of perioperative blood transfusion for liver resection. World J Surg 40(2481–248):9. https://doi.org/10.1007/s00268-016-3544-8
Pang Q, Qu K, Zhang JY et al (2015) The prognostic value of platelet count in patients with hepatocellular carcinoma: a systematic review and meta-analysis. Medicine (Baltimore) 94:e1431
Tung-Ping Poon R, Fan ST, Wong J (2000) Risk factors, prevention, and management of postoperative recurrence after resection of hepatocellular carcinoma. Ann Surg 232:10–24
Bagirsakci E, Sahin E, Atabey N et al (2017) Role of albumin in growth inhibition in hepatocellular carcinoma. Oncology 93(136–14):2
Nojiri S, Joh T (2014) Albumin suppresses human hepatocellular carcinoma proliferation and the cell cycle. Int J Mol Sci 15(5163–517):4
Acknowledgement
This study was supported by Grants from Science and Technological Supports Project of Sichuan Province (2016SZ0025 and 2015SZ0049) as well as Health and Family Planning Commission of Sichuan Province (17PJ393).
Author contributions
CL and TFW proposed this study. CL, WP, XYZ, LNY, BL, JYY, WTW, and MQX collected the data. CL and XYZ analyzed the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Li, C., Zhang, XY., Peng, W. et al. Postoperative Albumin–Bilirubin Grade Change Predicts the Prognosis of Patients with Hepatitis B-Related Hepatocellular Carcinoma Within the Milan Criteria. World J Surg 42, 1841–1847 (2018). https://doi.org/10.1007/s00268-017-4355-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4355-2