Abstract
Background
In hypotensive patients with thoracoabdominal penetrating injuries, trauma surgeons often face a considerable dilemma, which cavities and when to explore. We hypothesized that the Focused Assessment with Sonography for Trauma (FAST) would be accurate enough to determine the need and sequence of cavity exploration.
Methods
We conducted a 4-year retrospective study at a level 1 trauma center with high penetrating trauma volume. Patients with potential multi-cavity thoracoabdominal injuries were selected based on the location and number of external wounds. Findings in the operation or on computed tomography were used as references to evaluate the sensitivity, specificity, positive predictive value and negative predictive value of pericardial and abdominal FAST.
Results
A total of 2851 patients with penetrating injury were admitted from 2012 to 2015. Of those, 103 patients (3.6%) met our inclusion criteria (stab wounds 56.3%, gunshot wounds 43.7%). Median age: 32, male gender: 89.3%, median injury severity score: 17, in-hospital mortality rate: 11.7%. Thirty-seven patients (35.9%) required surgical exploration of more than one cavity. Although the pericardial FAST was falsely negative in only one case with large left hemothorax, all cardiac injuries were treated without delay (12/13, 92.3% sensitivity). Sensitivity and specificity of the abdominal FAST was 68.5 and 93.9%, respectively.
Conclusions
In hypotensive patients following penetrating thoracoabdominal injuries, the pericardial FAST was highly sensitive and could reliably determine the need to explore the pericardium. While positive findings of abdominal FAST warrant an exploratory laparotomy, negative abdominal FAST does not exclude the abdominal cavity as a bleeding source.
Similar content being viewed by others
Introduction
Despite recent advances in trauma care, the management of patients with penetrating thoracoabdominal injuries remains challenging as these patients often require exploration of more than one body cavity. Moreover, unless a surgical plan for the sequencing of exploration of body cavities is adequately formulated, hemodynamically unstable patients may experience compromised outcomes [1,2,3]. A management algorithm for these complex cases, the so-called double jeopardy , has yet to be developed [1].
Ultrasound has been performed to identify pericardial and intraabdominal fluid collections in trauma patients since the 1980s, and the Focused Assessment with Sonography for Trauma (FAST) was developed in the 1990s [4, 5]. As the FAST examination can be rapidly performed at the bedside by non-radiologists, it is currently incorporated as a part of initial trauma assessment [6]. Furthermore, the FAST is particularly useful in guiding the management of patients with possible penetrating cardiac injury and hemodynamically unstable patients with blunt abdominal injury [7,8,9,10,11,12]. It was reported that the sensitivity and specificity of FAST for these populations approaches nearly 100% [12].
In contrast, the role of FAST appears to be limited in patients with possible penetrating intraabdominal injury. Compared with blunt trauma patients, studies in penetrating trauma patients have reported a lower sensitivity and specificity of the abdominal FAST [13, 14]. However, a large majority of the studies that evaluated the accuracy of FAST in penetrating abdominal injury have excluded hemodynamically unstable patients because of the strong indication to proceed immediately with an abdominal exploration [10, 13,14,15]. Thus, the accuracy of abdominal FAST in hemodynamically unstable patients with penetrating injury remains unclear [16]. This uncertainty becomes clinically relevant in scenarios with possible penetrating injuries to multiple thoracoabdominal cavities, in which case the trauma surgeon must determine which body region requires exploration and when.
In the current study, we sought to evaluate the accuracy of the FAST (pericardial and abdominal examinations) to identify pericardial and intraabdominal fluid collection in hemodynamically unstable patients with penetrating thoracoabdominal injuries. We hypothesized that results of the FAST would be sufficiently accurate to determine the need and sequence of cavity exploration in unstable patients who may require exploration of multiple anatomical cavities.
Patients and methods
We conducted a single-center retrospective study at an academic level 1 trauma center with a high penetrating trauma volume. After approval by the Institutional Review Board of the University of Southern California, our institutional trauma registry was queried for the data between January 2012 and December 2015. We included hemodynamically unstable trauma patients, defined as any episodes of systolic blood pressure <90 mmHg in the Emergency Department (ED), who presented with external penetrating wounds to the torso (neck, chest, abdomen, flank and back). The number and locations of external wounds was used to identify patients with possible penetrating multi-cavity thoracoabdominal injuries (thoracic, pericardial and abdominal cavity). We excluded (1) patients who did not have any recorded episodes of hypotension (systolic blood pressure <90 mmHg) during their ED stay, (2) patients with missing results of the FAST examination, (3) patients without any signs of life upon arrival or with admission systolic blood pressure or heart rate reported as “0” and (4) injury mechanisms other than stab wounds (SW) or gunshot wounds (GSW).
Patient demographics, location and number of external penetrating wounds, Abbreviated Injury Scale (AIS), Injury Severity Score (ISS), findings on the pericardial and abdominal FAST, computed tomography (CT) of the chest/abdomen/pelvis, chest radiography (CXR), sequencing of operative procedures and intraoperative findings were collected from the trauma registry and medical records. Outcome variables collected were in-hospital mortality, hospital length of stay, intensive care unit (ICU) length of stay and ventilator days. Relevant variables were compared between patients with SWs and GSWs. Values are reported as percentages for categorical variables and as medians with interquartile range (IQR) for nonparametric continuous variables. Pearson’s Chi-square test or Fisher’s exact test were used to compare proportions for categorical variables and Mann–Whitney U test to compare medians for continuous nonparametric variables as appropriate. A value p < 0.05 was considered statistically significant.
During the study period, the FAST examination was performed (SonoSite S Series: FUJIFILM SonoSite Inc, Bothell, WA) and interpreted by PGY2-4 level emergency medicine residents under the supervision of an attending trauma surgeon and emergency medicine physician. The pericardial and abdominal FAST examinations were considered positive if free fluid was observed in the pericardial and intraabdominal space, respectively. Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of respective pericardial and abdominal FAST examinations were calculated in reference to intraoperative findings, results of CT and clinical observation during hospital stay (Table 1). Indications and sequences of emergent surgical interventions were determined at the discretion of attending trauma surgeons.
Results
A total of 2851 patients with penetrating injury were admitted during the study period. Of those, 103 (3.6%) met our inclusion and exclusion criteria (Fig. 1). Figure 2 is an illustration of the number and location of external penetrating wounds in the study population. The majority of wounds were located in the anterior chest (121 wounds), with more than 40% of which were located lateral to the left midclavicular line. A total of 77 wounds were documented in the anterior abdomen, followed by 62 wounds in the bilateral flank/back and 47 wounds in the posterior chest. Of 103 patients, 47 patients had >2 external wounds and 19 patients had 2 wounds. In 37 patients with one external wound, multi-cavity thoracoabdominal injuries were suspected based on the area of external wound, clinical and radiological findings (e.g., location of a bullet).
Patients with SW comprised 56.3% of the study population, while 43.7% sustained GSW (Table 2). The majority of the patients were male (89.3%), with a median age of 32 years (IQR 22–40.5). Median ISS was 17 (IQR 10–26). In 83 patients (80.6%), operative exploration was required in at least one body cavity. Exploratory laparotomy and pericardial exploration were performed in 68 (66%) and 33 patients (32%), respectively. Patients who sustained GSW were more likely to require an exploratory laparotomy compared with SW patients (86.7 vs. 50.0%, p < 0.001). However, there was no significant difference in the percentage of patients who required a pericardial exploration between two groups (37.8 vs. 27.6%, p = 0.27). Both laparotomy and pericardial exploration were required in 20 patients (19.4%) with a significantly higher rate in patients with GSW (33.3 vs. 8.6% p = 0.002). Overall in-hospital mortality rate was 11.7%, with a median hospital length of stay of 8 days (IQR 4.5–17.5).
Pericardial FAST was positive in 16 patients, all of whom underwent surgical exploration of the pericardium without further diagnostic tests. Cardiac injury was identified in 12 patients, whereas 3 patients had a negative exploration. Non-trauma-related pericardial effusion was found in one patient. Although other cavities were explored prior to the pericardium in 3 patients (2 abdomen and 1 left thorax), these patients all survived to discharge. Of 87 patients with negative pericardial FAST, chest CT was obtained in 5 patients. Pericardial FAST was falsely negative in one case with a large left hemothorax on chest CT following GSW. However, the pericardium was explored first and the cardiac injury was treated without further delay. The other 16 pericardial explorations were all negative.
Abdominal FAST was positive in 40 patients, 39 of whom underwent exploratory laparotomy, and 4 patients had CT of the abdomen/pelvis. Three patients with positive CT were then taken to the operating room for abdominal exploration. The other patient with positive CT underwent angioembolization for grade III liver lacerations. Of 63 patients with negative abdominal FAST, exploratory laparotomy was performed in 12 patients without abdominopelvic CT, 4 of whom had a positive laparotomy. Abdominopelvic CT was performed for further diagnostic workup in 37 patients. Of those, 13 patients were found to have intraabdominal free fluid on CT. Serial physical examinations and laboratory tests remained negative throughout the hospital course in 14 patients who did not undergo surgical exploration or CT. Abdominal and pericardial FAST examinations were both positive in 5 patients and both negative in 52 patients.
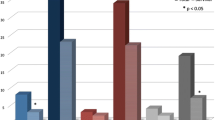
Sensitivity, specificity, PPV and NPV of the pericardial and abdominal FAST are shown in Fig. 3. Overall sensitivity and specificity for pericardial FAST was 92.3 and 95.6%, while sensitivity and specificity for abdominal FAST was 68.5 and 93.9%, respectively. Sensitivity of the pericardial FAST was 100% in the SW group. The pericardial FAST was also highly specific in both SW and GSW groups (94.0 and 97.5%, respectively). Sensitivities of the abdominal FAST were similar in the SW and GSW group (62.5 vs. 73.3%, p = 0.39). Specificity of the abdominal FAST was 100% in the SW group, whereas 3 false-positive cases were identified in the GSW group (12/15, specificity 80%).
Discussion
In patients with thoracoabdominal penetrating injuries, a rapid and accurate screening of each body cavity for active hemorrhage must be performed. With limited diagnostic modalities in the resuscitation bay, trauma surgeons have to make two critical decisions: location and timing of body cavity exploration [2]. These decisions are frequently misguided by findings in physical examination or chest tube output. Asensio et al. reported significantly high negative thoracotomy and laparotomy rates (13 and 11%, respectively) in their series of penetrating thoracoabdominal injuries [2]. More than half of negative laparotomies were performed because of injury mechanism. In another study conducted in the early 1990s when FAST was not routinely performed in trauma, incorrect sequencing of the primary operation occurred in 23% (19/81) of cases and 19% (10/81) had a negative laparotomy [1]. Of note, 4 patients died in the operating room during a negative cavitary exploration.
To our knowledge, this is the first study to evaluate the accuracy of the pericardial and abdominal FAST as an adjunct diagnostic test in hemodynamically unstable patients with possible penetrating, multi-cavity injuries. We found the pericardial FAST to be highly sensitive (92.3%) and specific (95.6%). The abdominal FAST was also very specific (93.9%), but less sensitive (68.5%). These data suggest that the FAST in hypotensive patients following penetrating trauma may be valuable in determining the need for exploration of the pericardial cavity, but less useful in ruling out intraabdominal hemorrhage. It is also important to note that the abdominal FAST’s high specificity makes it a valuable modality for confirming intraabdominal hemorrhage. We believe that although these strengths and weaknesses of the FAST require consideration, the FAST should become an integral part of management algorithm in unstable patients with penetrating thoracoabdominal injury.
Previous studies have suggested that of injuries to three anatomical cavities (pericardium, thorax and abdomen), accurate diagnosis of cardiac injury is the most critical cavity in regard to improved patient outcomes [1,2,3, 17, 18]. In 16 SW patients who required both laparotomy and thoracotomy, Clarke et al. [3] evaluated adherence to the proper sequence of surgical exploration. Of the 16 patients, cardiac injury was missed initially in all four cases where incorrect sequencing had occurred. Additionally, another study by Berg et al. [17, 18] reviewed all cases with thoracoabdominal penetrating injury at our institution over a 16-year period. Up to 70% of SW patients who underwent thoracotomy were found to have cardiac injury. Similarly, cardiac injury was identified in 25% of GSW patients who required a thoracotomy. Given the high rate of cardiac injury in penetrating trauma, the authors advocated the use of the pericardial FAST to exclude cardiac injury, particularly in SW patients. Identification of free fluid within the pericardium (hemopericardium) using pericardial FAST has been shown to be highly sensitive and specific in penetrating trauma patients. Both retrospective and prospective studies performed by Rozycki repeatedly showed 100% sensitivity of the pericardial FAST in patients with potential penetrating cardiac injury [7, 12]. Of note, authors from the same institution later reported five SW cases with false-negative pericardial FAST examinations from a total of 228 patients [19]. All five patients had associated left hemothorax which was caused by decompressed pericardial blood from a hole in the pericardium. One patient with a false-negative pericardial FAST in our current study was also found to have a similar injury pattern. Furthermore, Berg et al. reported that, in thoracoabdominal GSW patients with cardiac injury, up to 22% of patients had a false-negative pericardial FAST due to associated diaphragm injury and upper abdominal solid organ injuries [18]. Thus, it is very important to evaluate multiple body cavities (pericardium, bilateral thorax and abdomen) as sources of active hemorrhage in the management of hypotensive patients with penetrating torso injury.
The FAST has also been proven to be a powerful diagnostic tool to identify intraabdominal hemorrhage in hypotensive patients with blunt torso injury [8,9,10,11]. In other words, exploratory laparotomy is strongly indicated when these patients are found to have a positive abdominal FAST. An early study by Rozycki et al. showed 100% sensitivity and specificity of the abdominal FAST to identify free fluid in the abdomen (hemoperitoneum) in 30 blunt trauma patients with hemodynamic instability. However, its sensitivity was decreased to 75.7% in 1129 normotensive patients [12]. In contrast, the utility of abdominal FAST has been questioned in penetrating trauma [13, 14, 20,21,22]. In a multi-center prospective study, Biffl et al. [20] reported that less than a half of anterior abdominal stab wound (AASW) patients without indications for an emergent laparotomy (hypotension, peritonitis, or evisceration) underwent the abdominal FAST. Furthermore, the management decision was made based on the FAST results in only 4% of patients who underwent the abdominal FAST. Of note, 23% of study patients with a negative abdominal FAST still required a therapeutic laparotomy due to the high incidence of hollow viscus injuries in penetrating injury. On the other hand, 28% of patients with a positive FAST did not require a therapeutic laparotomy. Routine use of the abdominal FAST is, therefore, not currently recommended in hemodynamically stable patients with AASW. Similarly, the FAST is not commonly used for the decision-making process in hemodynamically unstable patients with isolated penetrating abdominal injury as these patients require an immediate laparotomy irrespective of the FAST result. Our data agree that a negative abdominal FAST cannot safely rule out intraabdominal hemorrhage in patients with potential multi-cavity penetrating injuries. Approximately 30% of patients with negative abdominal FAST were found to have hemoperitoneum in subsequent laparotomy or on CT. Nonetheless, it is also important to note that our data showed the PPV of the abdominal FAST was very high, particularly in SWs patients. Thus, in patients with negative pericardial FAST and unremarkable chest radiography, a positive abdominal FAST should be considered as a strong indication for emergent laparotomy.
There are several limitations to the current study. First, due to its retrospective nature, we were not able to determine how strongly the FAST results impacted the decision-making processes. This was particularly true in the case of the patient who underwent multi-cavity explorations (thorax, pericardium and abdomen), as we were unable to determine whether sequencing of operative intervention was determined based on the FAST findings. Similarly, sequelae of false-positive/false-negative FAST need to be evaluated in a future prospective study. Second, as this is a single-center study, our results may not be applicable to other institutions. Significant disparities may exist in the use of the FAST for penetrating trauma at different trauma centers. Our institution had not implemented the protocol for recording all FAST images until 2015. Therefore, all FAST results were collected by reviewing medical records. Although our data need to be validated in a multi-center study, we believe that all FAST examinations evaluated were performed by adequately trained physicians in a standard fashion as the FAST is commonly performed by non-radiologists in the USA [21]. Lastly, our protocol did not include an additional thoracic examination during the study period. Portable chest radiography was performed to look for significant intrathoracic injuries in most of our cases. As previous studies reported high sensitivities and specificities of thoracic ultrasound for identifying pneumothorax and hemothorax in trauma [23, 24], the utility of extended FAST (E-FAST) should be evaluated in penetrating trauma. Even with these limitations, the study provides some of the first data showing how FAST can be better utilized to treat hypotensive patients with thoracoabdominal penetrating injuries, allowing the surgeon to prioritize which cavities, if any, need to be opened and explored for hemorrhage control. The FAST is an examination performed worldwide, and the findings here can be readily translated into clinical practice with minimal changes to existing hospital protocols. Though CT provides more detailed information about thoracoabdominal injuries, ultrasound’s superior speed and ease of access give it a role even in urgent situations where standard of care dictates taking the patient directly to the operating room. A better understanding of the sensitivity and specificity of the imaging in these clinical scenarios can help physicians make better, more informed decisions.
Conclusions
In unstable patients with penetrating thoracoabdominal injuries, our data suggest that the pericardial FAST has excellent sensitivity and specificity when assessing for the need to explore the pericardial cavity. While the abdominal FAST is not sensitive enough to be used as a screening test for intraabdominal hemorrhage, its high specificity for abdominal hemorrhage also makes it useful for ruling in a bleeding source in the abdominal cavity. The ready availability and affordability of the FAST make it a powerful modality, and a better understanding of its strengths and weaknesses will translate into better clinical practice in the future.
References
Hirshberg A, Wall MJ Jr, Allen MK et al (1995) Double jeopardy: thoracoabdominal injuries requiring surgical intervention in both chest and abdomen. J Trauma 39:225–229
Asensio JA, Arroyo H Jr, Veloz W et al (2002) Penetrating thoracoabdominal injuries: ongoing dilemma-which cavity and when? World J Surg 26:539–543. doi:10.1007/s00268-001-0147-8
Clarke DL, Gall TM, Thomson SR (2011) Double jeopardy revisited: clinical decision making in unstable patients with, thoraco-abdominal stab wounds and potential injuries in multiple body cavities. Injury 42:478–481
Kimura A, Otsuka T (1991) Emergency center ultrasonography in the evaluation of hemoperitoneum: a prospective study. J Trauma 31:20–23
Scalea TM, Rodriguez A, Chiu WC et al (1999) Focused Assessment with Sonography for Trauma (FAST): results from an international consensus conference. J Trauma 46:466–472
The American College of Surgeons (2012) Advanced trauma life support student course manual, 9th edition
Rozycki GS, Feliciano DV, Schmidt JA et al (1996) The role of surgeon-performed ultrasound in patients with possible cardiac wounds. Ann Surg 223:737–746
McKenney MG, Martin L, Lentz K et al (1996) 1000 consecutive ultrasounds for blunt abdominal trauma. J Trauma 40:607–612
Ma OJ, Mateer JR, Ogata M et al (1995) Prospective analysis of a rapid trauma ultrasound examination performed by emergency physicians. J Trauma 38:879–885
Rozycki GS, Ochsner MG, Schmidt JA et al (1995) A prospective study of surgeon-performed ultrasound as the primary adjuvant modality for injured patient assessment. J Trauma 39:492–498
Lee BC, Ormsby EL, McGahan JP et al (2007) The utility of sonography for the triage of blunt abdominal trauma patients to exploratory laparotomy. AJR Am J Roentgenol 188:415–421
Rozycki GS, Ballard RB, Feliciano DV et al (1998) Surgeon-performed ultrasound for the assessment of truncal injuries: lessons learned from 1540 patients. Ann Surg 228:557–567
Udobi KF, Rodriguez A, Chiu WC et al (2001) Role of ultrasonography in penetrating abdominal trauma: a prospective clinical study. J Trauma 50:475–479
Soffer D, McKenney MG, Cohn S et al (2004) A prospective evaluation of ultrasonography for the diagnosis of penetrating torso injury. J Trauma 56:953–957
Boulanger BR, Kearney PA, Tsuei B et al (2001) The routine use of sonography in penetrating torso injury is beneficial. J Trauma 51:320–325
Bank MA, Frankel HL, Tandon M et al (2004) Use of FAST to prioritize treatment of concomitant penetrating head, chest and torso wounds. Am J Emerg Med 22:491–492
Berg RJ, Karamanos E, Inaba K et al (2014) The persistent diagnostic challenge of thoracoabdominal stab wounds. J Trauma Acute Care Surg 76:418–423
Berg RJ, Inaba K, Okoye O, Karamanos E, Strumwasser A, Chouliaras K, Teixeira PG, Demetriades D (2014) The peril of thoracoabdominal firearm trauma: 984 civilian injuries reviewed. J Trauma Acute Care Surg 77:684–691
Ball CG, Williams BH, Wyrzykowski AD et al (2009) A caveat to the performance of pericardial ultrasound in patients with penetrating cardiac wounds. J Trauma 67:1123–1124
Biffl WL, Kaups KL, Cothren CC et al (2009) Management of patients with anterior abdominal stab wounds: a Western Trauma Association multicenter trial. J Trauma 66:1294–1301
Brooks A, Davies B, Smethhurst M et al (2004) Prospective evaluation of non-radiologist performed emergency abdominal ultrasound for haemoperitoneum. Emerg Med J 21:e5
Soto JA, Morales C, Múnera F et al (2001) Penetrating stab wounds to the abdomen: use of serial US and contrast-enhanced CT in stable patients. Radiology 220:365–371
Blaivas M, Lyon M, Duggal S (2005) A prospective comparison of supine chest radiography and bedside ultrasound for the diagnosis of traumatic pneumothorax. Acad Emerg Med 12:844–849
Kirkpatrick AW, Sirois M, Laupland KB et al (2004) Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the Extended Focused Assessment with Sonography for Trauma (EFAST). J Trauma 57:288–295
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Matsushima, K., Khor, D., Berona, K. et al. Double Jeopardy in Penetrating Trauma: Get FAST, Get It Right. World J Surg 42, 99–106 (2018). https://doi.org/10.1007/s00268-017-4162-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4162-9