Abstract
Background
We aimed to describe the pattern of solid organ injuries (SOIs) and analyze the characteristics, management and outcomes based on the multiplicity of SOIs.
Methods
A retrospective study in a Level 1 trauma center was conducted and included patients admitted with blunt abdominal trauma between 2011 and 2014. Data were analyzed and compared for patients with single versus multiple SOIs.
Results
A total of 504 patients with SOIs were identified with a mean age of 28 ± 13 years. The most frequently injured organ was liver (45%) followed by spleen (30%) and kidney (18%). One-fifth of patients had multiple SOIs, of that 87% had two injured organs. Patients with multiple SOIs had higher frequency of head injury and injury severity scores (p < 0.05). The majority of SOIs were treated nonoperatively, whereas operative management was required in a quarter of patients, mostly in patients with multiple SOIs (p = 0.01). Blood transfusion, sepsis and hospital stay were greater in multiple than single SOIs (p < 0.05). The overall mortality was 11% which was comparable between the two groups. In patients with single SOIs, the mortality was significantly higher in those who had pancreatic (28.6%) or hepatic injuries (13%) than the other SOIs.
Conclusion
SOIs represent one-tenth of trauma admissions in Qatar. Although liver was the most frequently injured organ, the rate of mortality was higher in pancreatic injury. Patients with multiple SOIs had higher morbidity which required frequent operative management. Further prospective studies are needed to develop management algorithm based on the multiplicity of SOIs.
Similar content being viewed by others
Introduction
Trauma is a major public health problem worldwide, especially in young adults, with an annual death rate of 5.8 million which is expected to reach 8.4 million by the year 2020 [1, 2]. Solid organ injuries (SOIs) following blunt abdominal trauma are often associated with significant morbidity and mortality. Motor vehicle crash (MVC) is the leading mechanism of blunt abdominal trauma [3,4,5,6]. These injuries account for 1 out of 7 blunt trauma admissions mainly SOIs involving liver and spleen [3]. Pancreatic injuries are rare and often coexist with other injuries [7]. The management of SOIs depends upon the hemodynamic status of the patients. Hemodynamically unstable patients require either damage control laparotomy and/or definitive surgery [8]. The damage control surgery refers to the invasive monitoring with cardiopulmonary support, aggressive rewarming, replacement of blood and clotting factors to correct the lethal triad of trauma, namely coagulopathy, hypothermia and acidosis [8]. Nonoperative management (NOM) is preferred in hemodynamically stable patients. Over the years, with the advancements in diagnostic modalities together with improved assessment of the grade or extent of injury, NOM has increased and becomes widely accepted approach [8]. NOM is usually preferred in patients with lower injury grade, as higher grade injuries are often associated with failure of NOM and more likely to be treated surgically [9]. Frequent concomitant injuries, need for blood transfusion, higher serum lactate level and Sequential Organ Failure Assessment (SOFA) score are observed in patients with multiple SOIs [9]. Notably, the success of NOM, postoperative complications and mortality depends on the involvement of SOIs, i.e., single or multiple organ injuries [9]. Therefore, the current study was undertaken to describe the pattern of SOIs and to compare the characteristics, management and outcomes based on the multiplicity of SOIs in patients’ sustained blunt abdominal trauma.
Methods
This retrospective study was based on a prospectively collected trauma registry database in the only level 1 Hamad Trauma Center (HTC) in Qatar, over a period of 3 years (June 2011–June 2014). The study included all patients admitted with SOIs (liver, spleen, kidney and pancreas) following blunt abdominal trauma. Patients with penetrating injuries were excluded from the study.
We collected data on demographics, mechanism of injury, SOIs, associated injuries, comorbidities, organ injury grades, severity of injury (as expressed by injury severity score, Glasgow Coma score (GCS), abbreviated injury scores), initial vitals, radiological findings, diagnostic work-up, blood transfusion, management (NOM or OM), hospital course (complications, length of ICU and hospital stay, ventilatory days) and outcome.
All hemodynamically stable patients presented with abdominal trauma or had positive Focused Assessment with Sonography for Trauma (FAST) on admission underwent abdominal computerized tomography (CT) scanning. The management of patients with SOI is primarily considered based on the physiological status and injury grades. All hemodynamically stable patients are transferred to the trauma intensive care unit (TICU) for NOM which includes serial clinical assessment and laboratory investigations. Angioembolization is considered as adjunct to NOM, if the CT scan finding indicates an arterial blush. Follow-up CT scanning is considered for high-grade SOIs, those underwent angioembolization and had evidence of continuous bleeding with drop in hemoglobin level or if an associated hollow viscus injury is suspected.
The operative management (OM) is considered for patient presenting with hemorrhagic shock and had positive FAST, deteriorated clinically or failed NOM. There is no specific protocol for the “failure of NOM,” and the decision to shift for the OM depends on the discretion of treating physician. Patients are considered hemodynamically unstable with a drop in systolic blood pressure of more than 30 mmHg and hypotension (systolic blood pressure (SBP) under 90 mmHg) in spite of adequate fluid resuscitation. The diagnosis and grading of SOIs are either based on CT scan and/or intra-operative findings. The grading of SOIs is based on criteria of Organ Injury Scale established by American Association for the Surgery of Trauma (AAST) [10, 11]. Ethical approval was obtained from the Medical Research Center (IRB number 14409/14) at Hamad Medical Corporation, Doha, Qatar.
Statistical analysis
Data were presented as proportions, mean ± standard deviation (SD) or median as appropriate. Patients with single SOI were compared for associated injuries, intervention, and outcomes using Pearson Chi-square test for categorical variables and One-way ANOVA for continuous variables. Also, the baseline demographics, clinical presentation, management and outcomes were compared according to the involvement of SOI (single organ injury versus multiple organ injury) using the Student’s t test for continuous variables and Pearson Chi-square test for categorical variables. The Fisher’s exact test was used, if the expected cell frequencies were below five. For skewed continuous data, nonparametric Mann–Whitney test and Kruskal–Wallis test were performed. Multivariate logistic regression analysis was performed for the predictors of hospital mortality, and data were expressed as odd ratio (OR) and 95% confidence intervals (CI) utilizing the most relevant variables. Two-tailed p value < 0.05 was considered to be statistically significant. Data analysis was carried out using the Statistical Package for Social Sciences version 18 (SPSS Inc., Chicago, IL, USA).
Results
Patient characteristics
Of the total 4500 patients admitted with blunt trauma over 3 years, 504 (11.2%) sustained solid organ injuries. The majority were males (88%) with a mean age of 28.6 ± 13.2 years (Table 1). The most common mechanisms of injury were MVC (71%) and fall from height (19%). Rib fracture (43%), head injury (32%) and lung contusion (30%) were the frequently observed associated injuries. The mean GCS was 12 ± 4.9, and ISS was 19.6 ± 11.2. The mean AIS for head, chest and abdomen was 3.6 ± 1.1, 2.8 ± 0.7 and 2.6 ± 0.9, respectively.
Overall management and in-hospital outcomes
The majority of patients underwent abdominal CT scan (90%) evaluation and one-fourth was FAST positive. One hundred fourteen patients (23%) underwent exploratory laparotomy due to hypovolemic shock, and 390 (77%) were elected for NOM. Forty-one percent of the patients required blood transfusion.
Failure of NOM was observed in one patient with splenic injury who underwent splenectomy due to worsening abdominal pain and hypotension; the patient was successfully treated without postoperative complications. Moreover, seven patients of liver injury had failure of NOM of which one case underwent angioembolization.
Pneumonia (12%) was the most frequently reported complication followed by sepsis (6%). The median length of hospital stay, ICU stay and ventilatory support was 8 (1–304); 4 (1–69) and 3 (1–37) days, respectively. The overall mortality rate was 11% (55 deaths) (Table 2).
Distribution of SOIs grades and multiplicity
The most frequently injured solid organ was liver (45%) followed by spleen (30%), kidney (18%) and pancreas (7%). Table 3 demonstrates the overall distribution of injury grades for different solid organs. Higher grade injuries (≥3) were less frequent in liver and splenic injuries. Grade VI liver injuries were not reported, whereas grade V injuries constituted 4% of the liver injuries. On the other hand, Grade V splenic injuries were documented in 11%.
Furthermore, most patients (79%) sustained single SOIs, of which, liver injuries (52%) were more frequent followed by single splenic (32%), kidney (12%) and pancreatic (4%) injuries. Twenty-one percent (n = 108) patients had multiple SOIs, of which 13% had > two SOIs and 87% had two SOIs. Patients with more than two SOIs had higher frequency of combined liver, spleen and kidney (64.3%) injuries, whereas patients with two SOIs showed more frequent involvement of the liver & spleen (27.6%), liver & kidney (29.8%) and spleen & kidney (25.5%) injuries.
The associated injuries, intervention and outcomes in patients with single SOI are given in Table 4. Although the pancreas was the least single organ injured, patients with such injuries required frequent blood transfusion treated more with OM and had higher association with bowel injuries, sepsis and mortality in comparison with the other single SOIs. Blood transfusion was required more in patients who were treated surgically than those who did not (85.5 vs. 28.5%, p = 0.001) and the mean blood units was 12(± 10) versus 6(± 8), p = 0.001. Also blood transfusion was higher in patients with ISS > 15 (58.4%) than those who had lower ISS (14.6%), p = 0.001 and in patients with isolated splenic injury (41%) than liver injury (35%), p = 0.001.
Single versus multiple SOIs
The two groups were comparable with respect to age, gender, mechanism of injury and associated injuries, except for head injuries which were more frequent in patients with multiple SOIs (37% vs. 27%, p = 0.03). In comparison with single SOI group, patients in the multiple SOI group had lower mean GCS at ED (11.1 ± 5.2 vs. 12.3 ± 4.8, p = 0.04) and higher ISS (24.2 ± 12.2 vs. 18.5 ± 10.6, p = 0.001) (Table 5).
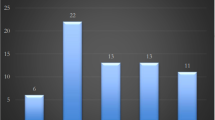
The operative management was more frequently performed in multiple SOIs (31 vs. 20%, p = 0.01). Similarly, endotracheal intubation, blood transfusion and chest tube insertion were done more often in multiple SOIs (p = 0.001). However, the frequency of ORIF for associated fractures was comparable (p = 0.66). Multiple SOIs group was more severely injured with higher rates of pneumonia and sepsis and had longer hospital and ICU stay (p < 0.05) when compared with patients with single SOI, albeit there was no significant difference in terms of in-hospital mortality between the two groups (10.6 vs. 12%, p = 0.59) (Table 5). In SOIs, the mortality was greater in patients with head injury (25.7 vs. 4.6%) than those without head injury. Figure 1 shows the mortality in each single SOI with the absence of head injury.
Multivariate regression analysis
After adjusting for age, ISS, abdominal AIS, GCS and SBP on admission, transfused blood units and exploratory laparotomy, the predictors of mortality were the ISS (OR 1.09; 95%CI 1.03–1.16), number of transfused blood units (OR 1.06; 95%CI 1.02–1.11), GCS (OR 0.77; 95%CI 0.78–0.88) and SBP (OR 0.97; 95%CI 0.95–0.98).
Discussion
The present study describes the pattern, management and outcomes of SOIs over a 3-year period in a small Middle Eastern country. This is a nationally representative study as all trauma patients are treated in the HTC which is the only level 1 trauma care facility in this country. The study shows that SOIs represent one-tenth of trauma admissions in Qatar. Notably, more than half of the single SOIs and 2 out of 3 multiple SOIs had involvement of liver injury which corresponds to the recent data suggesting that liver is the most commonly injured solid organ following blunt trauma [12]. The independent predictors of hospital mortality in our cohort were GCS at arrival, admission SBP, ISS and amount of PRBC transfused.
A high risk of single SOIs following abdominal trauma has been reported in previous studies. Malhotra et al. [13] studied blunt abdominal trauma patients admitted at two Level I trauma centers in the USA over a 4-year period. In comparison with our data, this study showed greater number of single SOIs (87%), higher proportion of MVCs-related injuries (80–88%) and lower proportion of fall from height (0.6–3%), whereas a study by Tinkoff et al. [14] which was based on the National Trauma Data Bank (NTDB) in the USA showed a lower proportion (66%) of single SOIs.
The male predominance and young age of injured patients in our study represent the actively mobile proportion of our population which is exposed to the risk for traumatic injuries particularly MVC and fall. In line with previous reports, our study demonstrated that MVC and falls lead the mechanism of injury in patients with SOIs [15]. However, neither MVCs nor falls have an impact on the multiplicity of SOIs in our study; as no significant association was observed with respect to the injury mechanism.
SOIs-associated injuries are crucial especially when the management options and outcomes are taken into account. In our study, the chest (ribs and lung) was the most frequently injured region followed by the head. Consistent with our findings, an earlier study showed more prevalence of chest injury in patients with hepatic trauma [16].
It has been suggested that higher organ injury severity grades are associated with adverse patient outcomes [17]. The distribution pattern of hepatic injury grades in our cohort is suggestive of mild injuries as only 4% of the total graded hepatic injuries sustained grade V injuries. Although relatively higher, a similar pattern of injury grades was also seen in patients with splenic injury. In contrast, Al-Qahtani et al. [18] reported a higher proportion of patients with grade IV splenic injuries (62%) from Saudi Arabia in comparison with only 11% in the present study. Of note, the sample size in that study was small with 61 splenic injury cases over a 9-year period.
In our cohort, single SOI patients were treated more frequently with NOM (79.8%). Similarly, Jeremitsky et al. [19] showed that more than 80% of the blunt splenic trauma patients had successful NOM, but it was more likely to fail in patients with higher injury grades. The majority of our single splenic injury patients who underwent NOM had lower grade of injuries. Blunt hepatic trauma patients were more likely to be stable, and therefore, NOM may significantly improve the outcomes when compared to the OM [16].
Evidence suggests that high ISS, head injury and blood transfusion requirements are crucial factors for the decision of OM and its outcomes [16, 20,21,22]. This is also evident from our study as OM was performed more frequently in patients with multiple SOIs presented with significantly higher ISS, associated head injury as well as the need for blood transfusion. In addition, these patients were more likely to develop complications such as pneumonia and sepsis and had prolonged hospital and ICU stay than the single SOI patients which corroborates with the findings of earlier studies [13, 16, 23].
In comparison with Malhotra et al. [13] study, the overall rate of failed NOM in our cohort was less (1.6 vs. 5%) which could be attributed to the predominance of single SOI and association of lower injury grades. Moreover, the mean ISS of patients within the single SOI group was relatively higher in Malhotra et al. (22 ± 13 vs. 19 ± 11) than that of our cohort.
The overall mortality in our study is 11% which is almost similar to Malhotra et al. [13] study but lower than that of Sawhney et al. [9] from India (15.6%). However, with respect to the multiple SOIs, the mortality was lower in our cohort (12%) in comparison with the previous study by Malhotra et al. (23%). Thirty-two percent of our cohort had head injury, whereas Malhotra et al. did not comment on such associated injuries.
Furthermore, mortality estimated in hepatic trauma patients from multiple studies was 10–19% which could be attributed to the injury grade, associated injuries and physiological characteristics of the patients [15, 16, 24, 25], whereas the mortality estimated from blunt splenic trauma ranged between 2 and 18% [19, 26].
Al-Qahtani et al. [18] demonstrated that the occurrence of bronchopneumonia, renal failure, and hypovolemic shock were associated with increased risk of mortality.
Interestingly, our study showed that single pancreatic SOI was associated with greater proportion of bowel injuries, operative intervention, development of sepsis and mortality (even in the absence of traumatic brain injury) in comparison with the other single SOIs. However, pancreatic injury was the least injured solid organ in our cohort. The pancreas is estimated to be the 10th most injured organ. The isolated type of pancreatic injury may occur in 0.2–0.7% of all abdominal injuries whereas it represents 21% of all the pancreatic injuries [27, 28]. Internal bleeding from associated vascular injury is a frequent cause of death in patients with a pancreatic trauma. However, the mortality rate is low even in severe injury (3–23%) as reported in earlier studies [27, 28].
Limitations
The present study has an inherent limitation and bias due to its retrospective design. The analysis was based on a registry data, and so there is a possibility of missing operative details and lack of information on missed diagnosis which could have impacted the data accuracy. Details of the management options in single pancreas or kidney were not included. Furthermore, we do not have long-term follow-up data to document any delayed postoperative complications and outcome. Additionally, the details of failed NOM in those who had multiple SOIs were not well defined and so we cannot comment on the association between the SOI multiplicity and NOM failure. Although blood transfusion was required in 41% of our patients, of which the majority were having multiple SOIs, we could not address where the blood transfusion was initiated. This observation deserves further assessment in prospective studies.
Conclusions
SOIs represent 11.2% of all trauma admissions with three-quarter of them have single SOIs. Liver with different injury grades is the most frequently injured organ; however, the mortality was greater in patients with pancreatic injury. OM was required more in patients with multiple SOIs than those with single SOI. Most SOI patients with hemodynamically stable status can be successfully managed nonoperatively. Associate head injury, ISS and hemodynamic stability play important prognostic role for mortality. Multiplicity of SOI is associated with higher morbidity and longer hospital care. However, further prospective studies are needed to inform the management algorithm in regard to SOI multiplicity.
References
Mock C, Lormand JD, Goosen J, et al (2004). Guidelines for essential trauma care. Geneva, World Health Organization. Retrieved from http://apps.who.int/iris/bitstream/10665/42565/1/9241546409_eng.pdf Accessed on 28 Jan 2017
Păun S, Beuran M, Negoi I et al (2011) Trauma–epidemiology: where are we today? Chirurgia (Bucur) 106:439–443
El-Menyar A, Abdelrahman H, Al-Thani H et al (2014) Compartmental anatomical classification of traumatic abdominal injuries from the academic point of view and its potential clinical implication. J Trauma Manag Outcomes 8:14. doi:10.1186/1752-2897-8-14 eCollection
Bergeron E, Lavoie A, Belcaid A et al (2007) Surgical management of blunt thoracic and abdominal injuries in Quebec: a limited volume. J Trauma 62:1421–1426
Gad MA, Saber A, Farrag S et al (2012) Incidence, patterns, and factors predicting mortality of abdominal injuries in trauma patients. North Am J Med Sci 4:129–134
Roozenbeek B, Maas AI, Menon DK (2013) Changing patterns in the epidemiology of traumatic brain injury. Nat Rev Neurol 9:231–236
O’Reilly DA, Bouamra O, Kausar A (2015) The epidemiology of and outcome from pancreatoduodenal trauma in the UK, 1989–2013. Ann R Coll Surg Engl 97:125–130
Brooks AJ, Rowlands BJ (1999) Blunt abdominal injuries. Br Med Bull 55:844–855
Sawhney C, Kaur M, Gupta B et al (2014) Critical care issues in solid organ injury: review and experience in a tertiary trauma center. Saudi J Anaesth 8:S29–S35
Yoon W, Jeong YY, Kim JK et al (2005) CT in blunt liver trauma. Radiographics 25:87–104
Madoff DC, Denys A, Wallace MJ et al (2005) Splenic arterial interventions: anatomy, indications, technical considerations, and potential complications. Radiographics 25:S191–S211
Yanar H, Ertekin C, Taviloglu K et al (2008) Nonoperative treatment of multiple intra-abdominal solid organ injury after blunt abdominal trauma. J Trauma 64:943–948
Malhotra AK, Latifi R, Fabian TC et al (2003) Multiplicity of solid organ injury: influence on management and outcomes after blunt abdominal trauma. J Trauma 54:925–929
Tinkoff G, Esposito TJ, Reed J et al (2008) American Association for the Surgery of Trauma Organ Injury Scale I: spleen, liver, and kidney, validation based on the National Trauma Data Bank. J Am Coll Surg 207:646–655
Ahmed I, Beckingham IJ (2007) Liver trauma. Trauma 9:171–180
Malhotra AK, Fabian TC, Croce MA et al (2000) Blunt hepatic injury: a paradigm shift from operative to non-operative management in the 1990s. Ann Surg 231:804–813
Stassen NA, Bhullar I, Cheng JD et al (2012) Selective nonoperative management of blunt splenic injury: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg 73:S294–S300
Al-Qahtani MS (2004) The pattern and management outcomes of splenic injuries in the Assir region of Saudi Arabia. West Afr J Med 23:1–6
Jeremitsky E, Kao A, Carlton C et al (2011) Does splenic embolization and grade of splenic injury impact nonoperative management in patients sustaining blunt splenic trauma? Am Surg 77:215–220
Beardsley C, Gananadha S (2011) An overview of liver trauma. MSJA 3:5–10
Piper GL, Peitzman AB (2010) Current management of hepatic trauma. Surg Clin North Am 90:775–785
David Richardson J, Franklin GA, Lukan JK et al (2000) Evolution in the management of hepatic trauma: a 25 year perspective. Ann Surg 232:324–330
Schnuriger B, Inderbitzin D, Schafer M et al (2008) Concomitant injuries are an important determinant of outcome of high grade blunt hepatic trauma. BJS 96:104–110
Zago TM, Pereira BM, Nascimento B, et al (2013) Hepatic trauma: a 21-year experience. Rev Col Bras Cir [periódico na Internet] 40(4). Disponível em http://www.scielo.br/rcbc
Hurtuk M, Reed RL 2nd, Esposito TJ et al (2006) Trauma surgeons practice what they preach: the NTDB story on solid organ injury management. J Trauma 61:243–255
El-Matbouly M, Jabbour G, El-Menyar A et al (2016) Blunt splenic trauma: assessment, management and outcomes. Surgeon 14:52–58. doi:10.1016/j.surge.2015.08.001
Siboni S, Kwon E, Benjamin E et al (2016) Isolated blunt pancreatic trauma: a benign injury? J Trauma Acute Care Surg 81:855–859
Hasanovic J, Agic M, Rifatbegovic Z et al (2015) Pancreatic injury in blunt abdominal trauma. Med Arch 69:130–132
Acknowledgements
We would like to thank all the database registry staff of the trauma section. This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector. All authors have read and approved the manuscript with no conflict of interest and no financial issues to disclose. Ethical approval was obtained from the Medical Research Center (IRB Number 14409/14) at Hamad Medical Corporation, Doha, Qatar. This study was presented in part at the World Trauma Congress, August 17–20, 2016, New Delhi, India.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest
Rights and permissions
About this article
Cite this article
El-Menyar, A., Abdelrahman, H., Al-Hassani, A. et al. Single Versus Multiple Solid Organ Injuries Following Blunt Abdominal Trauma. World J Surg 41, 2689–2696 (2017). https://doi.org/10.1007/s00268-017-4087-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4087-3