Abstract
Background
Although standard surgical treatment of stage I non-small cell lung cancer (NSCLC) is lobectomy, sublobar resection may be elected for small-sized (≤2 cm) peripheral tumors. Our aim was examine the need for completion lobectomy in the event of confirmed pleural or lymphovascular invasion after sublobar resection of NSCLC.
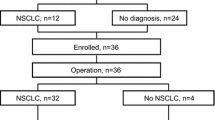
Methods
A total of 271 consecutive patients undergoing curative resection of stage I NSCLC ≤2 cm were reviewed retrospectively, analyzing clinicopathologic findings and survival times of those with invasion-positive (visceral pleural or lymphovascular invasion) or invasion-negative (neither visceral pleural nor lymphovascular invasion) tumors by surgical approach (sublobar resection vs lobectomy).
Results
Aside from age and pulmonary function, clinicopathologic characteristics of the patient subsets did not differ significantly, nor did 5-year recurrence-free survival rates of surgical subsets (sublobar resection vs lobectomy) in respective tumor groups (invasion-positive 78.9 vs 79.8%, p = 0.928; invasion-negative 80.2 vs 85.4%, p = 0.505). In multivariate analysis, dissected lymph node count was the sole parameter significantly impacting recurrence of stage I invasion-positive NSCLC (hazard ratio = 0.914, 95% confidence interval 0.845–0.988; p = 0.023). Sublobar resection was not a risk factor for recurrence.
Conclusions
Survival rates for patients with small-sized (≤2 cm) NSCLC and visceral pleural or lymphovascular invasion did not differ significantly, whether sublobar resection or lobectomy was done. Hence, completion lobectomy is unnecessary in this setting.




Similar content being viewed by others
References
Ginsberg RJ, Rubinstein LV (1995) Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group Ann Thorac Surg 60:615–622 discussion 622–613
Moon Y, Sung SW, Moon SW et al (2016) Risk factors for recurrence after sublobar resection in patients with small (2 cm or less) non-small cell lung cancer presenting as a solid-predominant tumor on chest computed tomography. J Thorac Dis 8:2018–2026
Okada M, Koike T, Higashiyama M et al (2006) Radical sublobar resection for small-sized non-small cell lung cancer: a multicenter study. J Thorac Cardiovasc Surg 132:769–775
Koike T, Kitahara A, Sato S et al (2016) Lobectomy Versus Segmentectomy in Radiologically Pure Solid Small-Sized Non-Small Cell Lung Cancer. Ann Thorac Surg 101:1354–1360
Cao C, Chandrakumar D, Gupta S et al (2015) Could less be more?-A systematic review and meta-analysis of sublobar resections versus lobectomy for non-small cell lung cancer according to patient selection. Lung Cancer 89:121–132
Blasberg JD, Pass HI, Donington JS (2010) Sublobar resection: a movement from the Lung Cancer Study Group. J Thorac Oncol 5:1583–1593
Nakamura K, Saji H, Nakajima R et al (2010) A phase III randomized trial of lobectomy versus limited resection for small-sized peripheral non-small cell lung cancer (JCOG0802/WJOG4607L). Jpn J Clin Oncol 40:271–274
Hung JJ, Jeng WJ, Hsu WH et al (2012) Predictors of death, local recurrence, and distant metastasis in completely resected pathological stage-I non-small-cell lung cancer. J Thorac Oncol 7:1115–1123
Park C, Lee IJ, Jang SH et al (2014) Factors affecting tumor recurrence after curative surgery for NSCLC: impacts of lymphovascular invasion on early tumor recurrence. J Thorac Dis 6:1420–1428
Mimae T, Tsutani Y, Miyata Y et al (2014) Role of lymphatic invasion in the prognosis of patients with clinical node-negative and pathologic node-positive lung adenocarcinoma. J Thorac Cardiovasc Surg 147:1820–1826
Kuo SW, Chen JS, Huang PM et al (2014) Prognostic significance of histologic differentiation, carcinoembryonic antigen value, and lymphovascular invasion in stage I non-small cell lung cancer. J Thorac Cardiovasc Surg 148(1200–1207):e1203
Mollberg NM, Bennette C, Howell E et al (2014) Lymphovascular invasion as a prognostic indicator in stage I non-small cell lung cancer: a systematic review and meta-analysis. Ann Thorac Surg 97:965–971
Lu P, Sun Y, Sun Y et al (2014) The role of (18)F-FDG PET/CT for evaluation of metastatic mediastinal lymph nodes in patients with lung squamous-cell carcinoma or adenocarcinoma. Lung Cancer 85:53–58
Moon Y, Kim KS, Lee KY et al (2016) Clinicopathologic Factors Associated With Occult Lymph Node Metastasis in Patients With Clinically Diagnosed N0 Lung Adenocarcinoma. Ann Thorac Surg 101:1928–1935
Edge SB, Byrd DR, Compton CC et al (2010) AJCC cancer staging manual. Springer, New York
Taioli E, Yip R, Olkin I et al (2016) Survival after sublobar resection for early-stage lung cancer: methodological obstacles in comparing the efficacy to lobectomy. J Thorac Oncol 11:400–406
Tao H, Hayashi T, Sano F et al (2013) Prognostic impact of lymphovascular invasion compared with that of visceral pleural invasion in patients with pN0 non-small-cell lung cancer and a tumor diameter of 2 cm or smaller. J Surg Res 185:250–254
Moon Y, Sung SW, Namkoong M et al (2016) The effectiveness of mediastinal lymph node evaluation in a patient with ground glass opacity tumor. J Thorac Dis 8:2617–2625
De Leyn P, Dooms C, Kuzdzal J et al (2014) Revised ESTS guidelines for preoperative mediastinal lymph node staging for non-small-cell lung cancer. Eur J Cardiothorac Surg 45:787–798
Heineman DJ, Ten Berge MG, Daniels JM et al (2016) Clinical Staging of Stage I Non-Small Cell Lung Cancer in the Netherlands-Need for Improvement in an Era with Expanding Nonsurgical Treatment Options: Data From the Dutch Lung Surgery Audit. Ann Thorac Surg 102:1615–1621
Altorki NK, Kamel MK, Narula N et al (2016) Anatomical Segmentectomy and Wedge Resections Are Associated with Comparable Outcomes for Patients with Small cT1N0 Non-Small Cell Lung Cancer. J Thorac Oncol 11:1984–1992
Acknowledgements
No specific grants from public, commercial, or nonprofit agencies funded this research. A native English-speaking professional (BioMed Proofreading, LLC) refined the written content.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Moon, Y., Lee, K.Y. & Park, J.K. Prognosis After Sublobar Resection of Small-sized Non-small Cell Lung Cancer with Visceral Pleural or Lymphovascular Invasion. World J Surg 41, 2769–2777 (2017). https://doi.org/10.1007/s00268-017-4075-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4075-7