Abstract
Background
To compare selected outcomes (30-day reoperation and total length of hospital stay) following emergency appendectomy between populations from New York State and England.
Methods
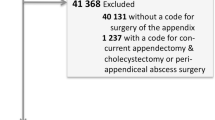
This retrospective cohort study used demographic and in-hospital outcome data from Hospital Episode Statistics (HES) and the New York Statewide Planning and Research Cooperative System (SPARCS) administrative databases for all patients aged 18+ years undergoing appendectomy between April 2009 and March 2014. Univariate and adjusted multivariable logistic regression were used to test significant factors. A one-to-one propensity score matched dataset was created to compare odd ratios (OR) of reoperations between the two populations.
Results
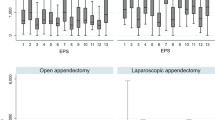
A total of 188,418 patient records, 121,428 (64.4%) from England and 66,990 (35.6%) from NYS, were extracted. Appendectomy was completed laparoscopically in 77.7% of patients in New York State compared to 53.6% in England (P < 0.001). The median lengths of hospital stay for patients undergoing appendectomy were 3 (interquartile range, IQR 2–4) days versus 2 (IQR 1–3) days (P < 0.001) in England and New York State, respectively. All 30-day reoperation rates were higher in England compared to New York State (1.2 vs. 0.6%, P < 0.001), representing nearly a twofold higher risk of 30-day reoperation (OR 1.88, 95% CI 1.64–2.14, P < 0.001). As the proportion of appendectomy completed laparoscopically increased, there was a reduction in the reoperation rate in England (correlation coefficient −0.170, P = 0.036).
Conclusions
Reoperations and total length of hospital stay is significantly higher following appendectomy in England compared to New York State. Increasing the numbers of appendectomy completed laparoscopically may decrease length of stay and reoperations.


Similar content being viewed by others
References
Buckius MT, McGrath B, Monk J, Grim R, Bell T, Ahuja V (2012) Changing epidemiology of acute appendicitis in the United States: study period 1993–2008. J Surg Res 175(2):185–190
Hospital Episode Statistics Admitted patient care–England 2011–2012. Total procedures and interventions. http://www.hscic.gov.uk/catalogue/PUB08288/hosp-epis-stat-admi-tot-ops-11-12-tab.xls
Ham C (2005) Money can’t buy you satisfaction. BMJ 330(7491):597–599
Klein R (1991) Risks and benefits of comparative studies: notes from another shore. Milbank Q 69(2):275–291
McGrath B, Buckius MT, Grim R, Bell T, Ahuja V (2011) Economics of appendicitis: cost trend analysis of laparoscopic versus open appendectomy from 1998 to 2008. J Surg Res 171(2):e161–e168
Schoen C, Davis K, How SKH, Schoenbaum SC (2006) U.S. health system performance: a national scorecard. Health Aff 25(6):w457–w475
Wennberg JE (2011) Time to tackle unwarranted variations in practice. BMJ 342
Kroon HM, Breslau PJ, Lardenoye JW (2007) Can the incidence of unplanned reoperations be used as an indicator of quality of care in surgery? Am J Med Qual 22(3):198–202
Birkmeyer JD, Hamby LS, Birkmeyer CM, Decker MV, Karon NM, Dow RW (2001) IS unplanned return to the operating room a useful quality indicator in general surgery? Arch Surg 136(4):405–411
Burns EM, Bottle A, Aylin P, Darzi A, Nicholls RJ, Faiz O (2011) Variation in reoperation after colorectal surgery in England as an indicator of surgical performance: retrospective analysis of Hospital Episode Statistics. BMJ 343
Gordon TA, Burleyson GP, Tielsch JM, Cameron JL (1995) The effects of regionalization on cost and outcome for one general high-risk surgical procedure. Ann Surg 221(1):43–49
Turrentine FE, Denlinger CE, Simpson VB, Garwood RA, Guerlain S, Agrawal A et al (2015) Morbidity, mortality, cost, and survival estimates of gastrointestinal anastomotic leaks. J Am Coll Surg 220(2):195–206
Lawson EH, Hall BL, Louie R, Ettner SL, Zingmond DS, Han L et al (2013) Association between occurrence of a postoperative complication and readmission: implications for quality improvement and cost savings. Ann Surg 258(1):10–18
van Walraven C, Jennings A, Forster AJ (2012) A meta-analysis of hospital 30-day avoidable readmission rates. J Eval Clin Pract 18(6):1211–1218
Jencks SF, Williams MV, Coleman EA (2009) Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 360(14):1418–1428
Moghadamyeghaneh Z, Hwang G, Hanna MH, Carmichael JC, Mills S, Pigazzi A et al (2016) Unplanned readmission after appendectomy. Am J Surg 212(3):493–500
Ramly EP, Bohnen JD, Farhat MR, Razmdjou S, Mavros MN, Yeh DD et al (2016) The nature, patterns, clinical outcomes, and financial impact of intraoperative adverse events in emergency surgery. Am J Surg 212(1):16–23
Nikkel LE, Kates SL, Schreck M, Maceroli M, Mahmood B, Elfar JC (2015) Length of hospital stay after hip fracture and risk of early mortality after discharge in New York state: retrospective cohort study. BMJ 351:h6246
Kocher RP, Adashi EY (2011) Hospital readmissions and the affordable care act: paying for coordinated quality care. JAMA 306(16):1794–1795
Fair BA, Kubasiak JC, Janssen I, Myers JA, Millikan KW, Deziel DJ et al (2015) The impact of operative timing on outcomes of appendicitis: a National Surgical Quality Improvement Project analysis. Am J Surg 209(3):498–502
National Surgical Research Collaborative (2013) Multicentre observational study of performance variation in provision and outcome of emergency appendicectomy. Br J Surg 100(9):1240–1252
Slavin JP, Deakin M, Wilson R (2012) Surgical research and activity analysis using Hospital Episode Statistics. Ann R Coll Surg Engl 94(8):537–538
Armitage JN, van der Meulen JH (2010) Identifying co-morbidity in surgical patients using administrative data with the Royal College of Surgeons Charlson Score. Br J Surg 97(5):772–781
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Birkmeyer JD, Siewers AE, Finlayson EVA, Stukel TA, Lucas FL, Batista I et al (2002) Hospital volume and surgical mortality in the United States. N Engl J Med 346(15):1128–1137
Guller U, Hervey S, Purves H, Muhlbaier LH, Peterson ED, Eubanks S et al (2004) Laparoscopic versus open appendectomy: outcomes comparison based on a large administrative database. Ann Surg 239(1):43–52
Wei B, Qi C-L, Chen T-F, Zheng Z-H, Huang J-L, Hu B-G et al (2010) Laparoscopic versus open appendectomy for acute appendicitis: a metaanalysis. Surg Endosc 25(4):1199–1208
Sauerland S, Jaschinski T, Neugebauer EA (2010) Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev (10):CD001546
American College of Surgeons Statements on principles. https://www.facs.org/about-acs/statements/stonprin
Mullen MG, Salerno EP, Michaels AD, Hedrick TL, Sohn M-W, Smith PW et al (2016) Declining operative experience for junior-level residents: is this an unintended consequence of minimally invasive surgery? J Surg Educ 73(4):609–615
Fahrner R, Schöb O (2012) Laparoscopic appendectomy as a teaching procedure: experiences with 1197 patients in a community hospital. Surg Today 42(12):1165–1169
SCOAP Collaborative, Cuschieri J, Florence M, Flum DR, Jurkovich GJ, Lin P, et al (2008) Negative appendectomy and imaging accuracy in the Washington State Surgical Care and Outcomes Assessment Program. Ann Surg. 248(4):557–563
Bhangu A, Begaj I, Ray D (2014) Population level analysis of diagnostic laparoscopy versus normal appendicectomy for acute lower abdominal pain. Int J Surg 12(12):1374–1379
Pritchard C, Wallace MS (2011) Comparing the USA, UK and 17 Western countries’ efficiency and effectiveness in reducing mortality. JRSM Short Rep 2(7):60
Lorence DP, Awad Ibrahim I (2003) Benchmarking variation in coding accuracy across the United States. J Health Care Financ 29(4):29–42
Parthasarathy M, Reid V, Pyne L, Groot-Wassink T (2015) Are we recording postoperative complications correctly? Comparison of NHS hospital episode statistics with the American college of surgeons national surgical quality improvement program. BMJ Qual Saf
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Al-Khyatt, W., Mytton, J., Tan, B.H.L. et al. A Population-Based Cohort Study of Emergency Appendectomy Performed in England and New York State. World J Surg 41, 1975–1984 (2017). https://doi.org/10.1007/s00268-017-3981-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-3981-z