Abstract
Background
Surgical readmissions have been extensively studied in North America, but very few data from other countries are available. We aimed to describe surgical readmissions in France and to assess their association with hospital status, surgical volume, and day surgery activity.
Methods
We performed a cross-sectional study encompassing all 1270 French hospitals, except for military hospitals and hospitals with very small volume. Data were retrieved from the national database regarding all patients undergoing surgery between January 1, 2010 and November 30, 2010. The main outcome measure was 30-day readmission rate. Association with hospital status, surgical volume, and the level of day surgery were assessed. Risk adjustment was performed based upon administrative categories.
Results
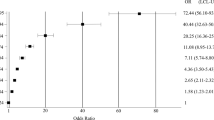
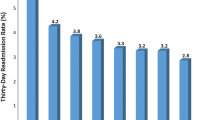
After exclusion of deaths and hospital transfers, there were 1,686,602 patients in the study cohort. Thirty-day readmission rate was 5.9 %. Distribution was skewed, with 21.5 % of procedures accounting for 33.5 % of all 30-day readmissions. Early readmissions (≤3 days) were associated with higher mortality as compared to those occurring later (>7 days) (3.2 vs. 2.6 %; p < 0.0001). After multivariate analysis, University hospitals were shown to be affected by a significantly greater risk of 30-day readmission as compared to private hospitals (odds ratio 1.46 [95 % CI 1.42–1.5]). Other independent factors were as follows: male gender, longer initial hospital stay, and comorbidities.
Conclusions
Surgical 30-day readmission rate was low, with early readmissions being associated with higher mortality. Conversely to prior research, University hospitals were shown to be associated with significantly higher risk of 30-day readmissions, even after risk adjustment.


Similar content being viewed by others
References
Joynt KE, Orav EJ, Jha AK (2011) Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA 305(675–68):1
Tsai TC, Orav EJ, Joynt KE (2014) Disparities in surgical 30-day readmission rates for Medicare beneficiaries by race and site of care. Ann Surg 259:1086–1090
Tsai TC, Joynt KE, Orav EJ et al (2013) Variation in surgical-readmission rates and quality of hospital care. N Engl J Med 369(1134–114):2
Krumholz HM, Lin Z, Keenan PS et al (2013) Relationship between hospital readmission and mortality rates for patients hospitalized with acute myocardial infarction, heart failure, or pneumonia. JAMA 309:587–593
Horwitz LI, Lin Z, Herrin J et al (2015) Association of hospital volume with readmission rates: a retrospective cross-sectional study. BMJ 350:h447
Dimick JB, Ghaferi AA (2015) Hospital readmission as a quality measure in surgery. JAMA 313(512–51):3
Tsai TC, Jha AK (2013) Surgical-readmission rates and quality of care. N Engl J Med 369(2460–246):1
Merkow RP, Ju MH, Chung JW et al (2015) Underlying reasons associated with hospital readmission following surgery in the United States. JAMA 313(483–49):5
Glance LG, Kellermann AL, Osler TM et al (2014) Hospital readmission after noncardiac surgery: the role of major complications. JAMA Surg 149(439–44):5
Morris MS, Deierhoi RJ, Richman JS et al (2014) The relationship between timing of surgical complications and hospital readmission. JAMA Surg 149(348–35):4
Joynt KE, Jha AK (2011) Who has higher readmission rates for heart failure, and why? Implications for efforts to improve care using financial incentives. Circ Cardiovasc Qual Outcomes 4:53–59
Hernandez AF, Greiner MA, Fonarow GC et al (2010) Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA 303:1716–1722
Parc Y, Reboul-Marty J, Lefevre JH, et al. (2015) Factors influencing mortality and morbidity following colorectal resection in France. Analysis of a national database (2009–2011). Colorectal Dis 18(2):205–213
Guerra J, Luciolli E, Felce A et al (2015) Data validity in a French diagnosis-related group information program. Rev Epidemiol Sante Publique 63:247–252
Author’s contribution
Dr. Lefèvre, Dr. Zeitoun, and Ms. de Vaugrigneuse were responsible for the conception and design of this work. Dr. Reboul-Marty retrieved the data and structured them into an exploitable dataset. Dr. Reboul-Marty and Dr. Lefèvre conducted the statistical analysis. Dr. Zeitoun drafted the manuscript. All authors participated in the analysis and interpretation of the data and critically revised the manuscript for important intellectual content. All authors gave final approval of the current version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
This project was not supported by any external grants or funds. All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf. No conflict of interests related to this work needs to be disclosed. Dr. Zeitoun reports he serves as an Advisor for several consulting firms and communication companies in link with pharmaceutical industry (Cepton, Oliver Wyman, Roland Berger, McCann Healthcare, Omnicom, Grey Healthcare, Saatchi and Saatchi Healthcare, Sudler and Hennessey, TBWA, inVentiv Health France, Havas). He also reports collaboration with Mayoly-Spindler, Merck, Teva, and Menarini, unpaid consultancy for EY and Allurion Technologies, conducting workshops funded by Amgen and being invited to a French medical congress by AbbVie. He is an Advisor in House at The Family, an investment company located in London and Paris where he is responsible for start-ups dedicated to health care. Dr. Lefèvre reports that he received fees from Vifor Pharma and being invited to an international medical congress by Sanofi, Cheks, and Eumedica. Dr. Reboul-Marty and Ms. de Vaugrigneuse report that they have no financial link with any health industry.
Data sharing
All authors had full access to all of the data in the study (including statistical reports and tables) and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Rights and permissions
About this article
Cite this article
Lefèvre, J.H., Reboul-Marty, J., de Vaugrigneuse, S. et al. Readmissions After Surgery: A French Nationwide Cross-Sectional Study of 1,686,602 Procedures Performed in 2010. World J Surg 41, 31–38 (2017). https://doi.org/10.1007/s00268-016-3740-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3740-6