Abstract
Background
The Pringle maneuver, which is performed during liver surgery to reduce blood loss, may result in liver ischemia/reperfusion injury resulting in metabolic, immunological, and microvascular changes, which may lead to hepatocellular damage. The aim of this study was the investigation of the effects of N-acetylcysteine (NAC) and methylprednisolone (MET) in the modulation of liver warm ischemia during hepatic resection.
Methods
Forty-eight patients were enrolled in a pilot double-blind, randomized clinical trial. The patients received either NAC, MET, or placebo. The primary endpoint was the reduction in postoperative alanine aminotransferase and bilirubin. The secondary endpoint was the difference in morbidity and mortality.
Results
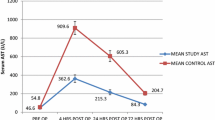
All the 48 patients had liver resection with no mortality. Morbidity was observed in 8 (16 %) patients equally distributed among the groups. There was a significant favorable recovery of liver function tests in patients treated with NAC or MET compared with the placebo when the Pringle maneuver exceeded 70 min.
Conclusions
The administration of NAC or MET prior to the Pringle maneuver during hepatic resection is associated with lower postoperative aberration in liver function tests compared with placebo when the Pringle maneuver exceeded 70 min. Larger studies are required to validate our findings and to investigate the specific role of NAC and MET in liver surgery.




Similar content being viewed by others
References
Jamieson GG, Corbel L, Campion JP et al (1992) Major liver resection without a blood transfusion: is it a realistic objective? Surgery 112:32–36
Kooby DA, Stockman J, Ben-Porat L et al (2003) Influence of transfusions on perioperative and long-term outcome in patients following hepatic resection for colorectal metastases. Ann Surg 237:860–870
Makuuchi M, Takayama T, Gunvén P et al (1989) Restrictive versus liberal blood transfusion policy for hepatectomies in cirrhotic patients. World J Surg 13:644–648. doi:10.1007/bf01658893
Torzilli G, Makuuchi M, Inoue K et al (1999) No-mortality liver resection for hepatocellular carcinoma in cirrhotic and noncirrhotic patients: is there a way? A prospective analysis of our approach. Arch Surg 134:984–992
Yamamoto J, Kosuge T, Takayama T et al (1994) Perioperative blood transfusion promotes recurrence of hepatocellular carcinoma after hepatectomy. Surgery 115:303–309
Pringle JH (1908) Notes on the arrest of hepatic hemorrhage due to trauma. Ann Surg 48:541–549
Imamura H, Kokudo N, Sugawara Y et al (2004) Pringle’s maneuver and selective inflow occlusion in living donor liver hepatectomy. Liver Transpl 10:771–778
Torzilli G, Procopio F, Donadon M et al (2012) Safety of intermittent Pringle maneuver cumulative time exceeding 120 minutes in liver resection: a further step in favor of the “radical but conservative” policy. Ann Surg 255:270–280
Glanemann M, Vollmar B, Nussler AK et al (2003) Ischemic preconditioning protects from hepatic ischemia/reperfusion-injury by preservation of microcirculation and mitochondrial redox-state. J Hepatol 38:59–66
Jaeschke H (2003) Molecular mechanisms of hepatic ischemia-reperfusion injury and preconditioning. Am J Physiol Gastrointest Liver Physiol 284:G15–G26
Serracino-Inglott F, Habib NA, Mathie RT (2001) Hepatic ischemia-reperfusion injury. Am J Surg 181:160–166
Kupiec-Weglinski JW, Busuttil RW (2005) Ischemia and reperfusion injury in liver transplantation. Transpl Proc 37:1653–1656
Ilmakunnas M, Tukiainen EM, Rouhiainen A et al (2008) High mobility group box 1 protein as a marker of hepatocellular injury in human liver transplantation. Liver Transpl 14:1517–1525
Abu-Amara M, Gurusamy K, Hori S et al (2010) Systematic review of randomized controlled trials of pharmacological interventions to reduce ischaemia-reperfusion injury in elective liver resection with vascular occlusion. HPB (Oxford) 12:4–14
Hayashi Y, Takayama T, Yamazaki S et al (2011) Validation of perioperative steroids administration in liver resection: a randomized controlled trial. Ann Surg 253:50–55
Jegatheeswaran S, Siriwardena AK (2011) Experimental and clinical evidence for modification of hepatic ischaemia-reperfusion injury by N-acetylcysteine during major liver surgery. HPB (Oxford) 13:71–78
McKay A, Cassidy D, Sutherland F et al (2008) Clinical results of N-acetylcysteine after major hepatic surgery: a review. J Hepatobiliary Pancreat Surg 15:473–478
Muratore A, Ribero D, Ferrero A et al (2003) Prospective randomized study of steroids in the prevention of ischaemic injury during hepatic resection with pedicle clamping. Br J Surg 90:17–22
Yamashita Y, Shimada M, Hamatsu T et al (2001) Effects of preoperative steroid administration on surgical stress in hepatic resection: prospective randomized trial. Arch Surg 136:328–333
Saidi RF, Chang J, Verb S et al (2007) The effect of methylprednisolone on warm ischemia-reperfusion injury in the liver. Am J Surg 193:345–347
Belghiti J, Clavien P, Gadzijev E et al (2000) The Brisbane 2000 terminology of liver anatomy and resections. HPB (Oxford) 2:333–339
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Schulz KF, Altman DG, Moher D (2010) CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 340:c332
Torzilli G, Procopio F, Costa G (2014) Resection guidance. In: Ultrasound-guided liver surgery: an atlas. Springer, New York, NY, pp 117–168
Donadon M, Costa G, Gatti A et al (2014) Thoracoabdominal approach in liver surgery: how, when, and why. Updates Surg 66:121–125
Torzilli G, Procopio F, Costa G (2014) Planning of the surgical strategy. In: Ultrasound-guided liver surgery: an atlas. Springer, New York, NY, pp 75–116
Gurusamy KS, Pamecha V, Sharma D et al (2009) Techniques for liver parenchymal transection in liver resection. Cochrane Database Syst Rev 1:Cd006880
Lesurtel M, Selzner M, Petrowsky H et al (2005) How should transection of the liver be performed?: a prospective randomized study in 100 consecutive patients: comparing four different transection strategies. Ann Surg 242:814–823
Takayama T, Makuuchi M, Kubota K et al (2001) Randomized comparison of ultrasonic vs clamp transection of the liver. Arch Surg 136:922–928
Torzilli G, Makuuchi M, Inoue K (2002) The vascular control in liver resection: revisitation of a controversial issue. Hepatogastroenterology 49:28–31
Donadon M, Costa G, Cimino M et al (2015) Diagnosis and management of bile leaks after hepatectomy: results of a prospective analysis of 475 hepatectomies. World J Surg 39:237–243. doi:10.1007/s00268-015-3143-0
Pulitanò C, Aldrighetti L, Arru M et al (2007) Prospective randomized study of the benefits of preoperative corticosteroid administration on hepatic ischemia-reperfusion injury and cytokine response in patients undergoing hepatic resection. HPB 9:183–189
Sugimoto T, Sozu T, Hamasaki T (2012) A convenient formula for sample size calculations in clinical trials with multiple co-primary continuous endpoints. Pharm Stat 11:118–128
Man K, Fan ST, Ng IO et al (1997) Prospective evaluation of Pringle maneuver in hepatectomy for liver tumors by a randomized study. Ann Surg 226:704–713
Belghiti J, Noun R, Malafosse R et al (1999) Continuous versus intermittent portal triad clamping for liver resection: a controlled study. Ann Surg 229:369–375
Elias D, Desruennes E, Lasser P (1991) Prolonged intermittent clamping of the portal triad during hepatectomy. Br J Surg 78:42–44
Makuuchi M, Mori T, Gunven P et al (1987) Safety of hemihepatic vascular occlusion during resection of the liver. Surg Gynecol Obstet 164:155–158
Kosuge T, Yamamoto J, Takayama T et al (1994) An isolated, complete resection of the caudate lobe, including the paracaval portion, for hepatocellular carcinoma. Arch Surg 129:280–284
Wu CC, Hwang CR, Liu TL et al (1996) Effects and limitations of prolonged ischaemia for hepatic resection of the cirrhotic liver. Br J Surg 83:121–124
Sakamoto Y, Makuuchi M, Takayama T et al (1999) Pringle’s maneuver lasting 322 min. Hepatogastroenterology 46:457–458
Ishizaki Y, Yoshimoto J, Miwa K et al (2006) Safety of prolonged intermittent Pringle maneuver during hepatic resection. Arch Surg 141:649–653
Procopio F, Torzilli G (2012) Forty-nine colorectal cancer liver metastases in one-stage hepatectomy with cumulative Pringle time lasting 348 min. Updates Surg 64:241–243
Ferrero A, Russolillo N, Vigano L et al (2010) Does Pringle maneuver affect survival in patients with colorectal liver metastases? World J Surg 34:2418–2425. doi:10.1007/s00268-010-0682-2
Giuliante F, Ardito F, Pulitano C et al (2010) Does hepatic pedicle clamping affect disease-free survival following liver resection for colorectal metastases? Ann Surg 252:1020–1026
Imamura H, Seyama Y, Kokudo N et al (2003) One thousand fifty-six hepatectomies without mortality in 8 years. Arch Surg 138:1198–1206
Sugiyama Y, Ishizaki Y, Imamura H et al (2010) Effects of intermittent Pringle’s manoeuvre on cirrhotic compared with normal liver. Br J Surg 97:1062–1069
Capussotti L, Muratore A, Ferrero A et al (2006) Randomized clinical trial of liver resection with and without hepatic pedicle clamping. Br J Surg 93:685–689
Hammond CL, Lee TK, Ballatori N (2001) Novel roles for glutathione in gene expression, cell death, and membrane transport of organic solutes. J Hepatol 34:946–954
McCord JM (1985) Oxygen-derived free radicals in postischemic tissue injury. N Engl J Med 312:159–163
Aruoma OI, Halliwell B, Hoey BM et al (1989) The antioxidant action of N-acetylcysteine: its reaction with hydrogen peroxide, hydroxyl radical, superoxide, and hypochlorous acid. Free Radic Biol Med 6:593–597
Zafarullah M, Li WQ, Sylvester J et al (2003) Molecular mechanisms of N-acetylcysteine actions. Cell Mol Life Sci 60:6–20
Kharazmi A, Nielsen H, Schiotz PO (1988) N-acetylcysteine inhibits human neutrophil and monocyte chemotaxis and oxidative metabolism. Int J Immunopharmacol 10:39–46
Majano PL, Medina J, Zubia I et al (2004) N-Acetyl-cysteine modulates inducible nitric oxide synthase gene expression in human hepatocytes. J Hepatol 40:632–637
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Donadon, M., Molinari, A.F., Corazzi, F. et al. Pharmacological Modulation of Ischemic-Reperfusion Injury during Pringle Maneuver in Hepatic Surgery. A Prospective Randomized Pilot Study. World J Surg 40, 2202–2212 (2016). https://doi.org/10.1007/s00268-016-3506-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3506-1