Abstract
Background
Perineal wound following abdominoperineal resection (APR) is associated with high complication rate and delayed healing. We aim to evaluate the risk factors for delayed wound healing and wound complications following APR.
Methods
A retrospective review of patients who underwent APR was performed. Non-delayed wound healing occurred within 6 weeks. Major complications included infection, necrosis, and dehiscence that required surgical interventions. Minor complications included drainage and superficial dehiscence that were treated conservatively. Patients were compared for type of wound closure (primary vs. flap reconstruction). Effect of patients’ demographic and clinical variables on time to healing, and on major and minor wound complications was examined.
Results
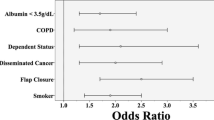
215 patients were identified, of which 175 (81 %) had primary closure and 40 (19 %) had flap reconstruction. Overall, major wound complications occurred in 14 (7 %) of patients and minor wound complications occurred in 48 (22 %). Mean time to wound healing was 6.3 weeks in the primary closure group and 9.3 weeks in the flap reconstruction group (p = 0.02). Delayed wound healing occurred in 44 (25 %) of the primary closure group and in 25 (62 %) of the flap reconstruction group (p < 0.001). Delayed wound healing was associated with smoking (p = 0.005), hypoalbuminemia (p = 0.05), neoadjuvant chemotherapy (p = 0.02), and flap reconstruction (p = 0.03). Hypoalbuminemia was associated with major wound complications (p = 0.002), while neoadjuvant chemotherapy was associated with minor wound complications (p = 0.01).
Conclusions
Wound complications and delayed healing are related to patients’ nutritional status, smoking, and neoadjuvant chemotherapy. Patients with these risk factors are at risk of delayed wound healing even if they underwent flap reconstruction.
Similar content being viewed by others
References
Miles WE (1908) A method of performing abdominal excision for carcinoma of the rectum and of the terminal portion of the pelvic colon. Lancet 2:1812–1813
Mauvais F, Sabbagh C, Brehant O et al (2011) The current abdominoperineal resection: oncological problems and surgical modifications for low rectal cancer. J Visc Surg 148:e85–e93
Shukla HS, Tewari M (2010) An evolution of clinical application of inferior pedicle based rectus abdominis myocutaneous flap for repair of perineal defects after radical surgery for cancer. J Surg Oncol 102:287–294
Holm T, Ljung A, Häggmark T et al (2007) Extended abdominoperineal resection with gluteus maximus flap reconstruction of the pelvic floor for rectal cancer. Br J Surg 94:232–238
West NP, Anderin C, Smith KJ et al (2010) Multicentre experience with extralevator abdominoperineal excision for low rectal cancer. European extralevator abdominoperineal excision study group. Br J Surg 97:588–599
Yu HC, Peng H, He XS et al (2014) Comparison of short- and long-term outcomes after extralevator abdominoperineal excision and standard abdominoperineal excision for rectal cancer: a systematic review and meta-analysis. Int J Colorectal Dis 29(2):183–191
West NP, Finan PJ, Anderin C et al (2008) Evidence of the oncologic superiority of cylindrical abdominoperineal excision for low rectal cancer. J Clin Oncol 26:3517–3522
Butler CE, Gündeslioglu AO, Rodriguez-Bigas MA (2008) Outcomes of immediate vertical rectus abdominis myocutaneous flap reconstruction for irradiated abdominoperineal resection defects. J Am Coll Surg 206(4):694–703
Tei TM, Stolzenburg T, Buntzen S et al (2003) Use of transpelvic rectus abdominis musculocutaneous flap for anal cancer salvage surgery. Br J Surg 90(5):575–580
Foster JD, Pathak S, Smart NJ et al (2012) Reconstruction of the perineum following extralevator abdominoperineal excision for carcinoma of the lower rectum: a systematic review. Colorectal Dis 9:1052–1059
Chan S, Miller M, Ng R et al (2010) Use of myocutaneous flaps for perineal closure following abdominoperineal excision of the rectum for adenocarcinoma. Colorectal Dis 12(6):555–560
Combs PD, Sousa JD, Louie O et al (2014) Comparison of vertical and oblique rectus abdominis myocutaneous flaps for pelvic, perineal, and groin reconstruction. Plast Reconstr Surg 134(2):315–323
Pang J, Broyles JM, Berli J et al (2014) Abdominal- versus thigh-based reconstruction of perineal defects in patients with cancer. Dis Colon Rectum 57(6):725–732
Chessin DB, Hartley J, Cohen AM et al (2005) Rectus flap reconstruction decreases perineal wound complications after pelvic chemoradiation and surgery: a cohort study. Ann Surg Oncol 12(2):104–110
Lefevre JH, Parc Y, Kernéis S et al (2009) Abdomino-perineal resection for anal cancer: impact of a vertical rectus abdominis myocutaneous flap on survival, recurrence, morbidity, and wound healing. Ann Surg 250(5):707–711
Arnold PG, Lovich SF, Pairolero PC (1994) Muscle flaps in irradiated wounds: an account of 100 consecutive cases. Plast Reconstr Surg 93(2):324–327
Kapoor V, Cole J, Isik FF et al (2005) Does the use of a flap during abdominoperineal resection decrease pelvic wound morbidity. Am Surg 71(2):117–122
Sorensen LT, Karlsmark T, Gottrup F (2003) Abstinence from smoking reduces incisional wound infection: a randomized controlled trial. Ann Surg 238(1):1–5
Kamrava A, Mahmoud N (2013) Prevention and management of nonhealing perineal wounds. Clin Colon Rectal Surg 26:106–111
Author contributions
Study concept, and design with data acquisition, analysis, and interpretation: Azah Althumairi, Joseph Canner, Jonathan Efron.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interests
None.
Additional information
This paper has been presented at the annual meeting of the American Society of Colon and Rectal Surgeons, Boston, MA, May 30–June 3, 2015.
Rights and permissions
About this article
Cite this article
Althumairi, A.A., Canner, J.K., Gearhart, S.L. et al. Predictors of Perineal Wound Complications and Prolonged Time to Perineal Wound Healing After Abdominoperineal Resection. World J Surg 40, 1755–1762 (2016). https://doi.org/10.1007/s00268-016-3450-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3450-0