Abstract
Background
The use of laparoscopic repair for perforated peptic ulcer (PPU) was shown to be safe and recommended in low-risk patients. However, whether the approach is safe to apply to high-risk patients is uncertain.
Study design
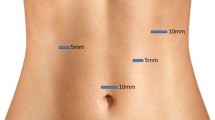
This was a retrospective study of all patients with PPU admitted between January 2002 and December 2012. The laparoscopy-first approach (LFA) was adopted as a routine for all patients. The outcomes of LFA for PPU were reviewed and assessed to determine if the approach was safe in high-risk patients.
Results
Three hundred and seventy three patients that suffered from PPU were included into the study and 50.9 % received laparoscopic repair. There was a significant increase in the number of operations performed yearly by the LFA (P < 0.001). 25.2 % of the patients had a Boey score of ≥2. High-risk patients that received LFA suffered from larger ulcers (P < 0.001) with more severe contamination (P = 0.006) that required conversion (P = 0.002) when compared to the low-risk patients. When compared to open surgery, more high-risk patients in the open group had ASA grade ≥3 (P = 0.007) and suffered from mortality (P = 0.001). The only significant predictor to mortality in high-risk patients was ASA grade ≥3 (P = 0.014).
Conclusions
The adoption of LFA in patients suffering from PPU was associated with acceptable rates of mortality and morbidity. The approach could also be selectively adopted in patients with Boey score ≥2 provided their ASA grading is low and hemodynamically stable.



Similar content being viewed by others
References
Lau JY, Sung J, Hill C, Henderson C, Howden CW, Metz DC (2011) Systematic review of the epidemiology of complicated peptic ulcer disease: incidence, recurrence, risk factors and mortality. Digestion 84:102–113
Ford AC, Delaney BC, Forman D, Moayyedi P (2006) Eradication therapy for peptic ulcer disease in Helicobacter pylori positive patients. Cochrane Database Syst Rev 2:CD003840
Ng EK, Lam YH, Sung JJ et al (2000) Eradication of Helicobacter pylori prevents recurrence of ulcer after simple closure of duodenal ulcer perforation: randomized controlled trial. Ann Surg 231:153–158
Bertleff MJ, Lange JF (2010) Perforated peptic ulcer disease: a review of history and treatment. Dig Surg 27:161–169
Lee FY, Leung KL, Lai PB, Lau JW (2001) Selection of patients for laparoscopic repair of perforated peptic ulcer. Br J Surg 88:133–136
Crofts TJ, Park KG, Steele RJ, Chung SS, Li AK (1989) A randomized trial of nonoperative treatment for perforated peptic ulcer. N Engl J Med 320:970–973
Lau WY, Leung KL, Kwong KH, Davey IC, Robertson C, Dawson JJ et al (1996) A randomized study comparing laparoscopic versus open repair of perforated peptic ulcer using suture or sutureless technique. Ann Surg 224:131–138
Bertleff MJ, Halm JA, Bemelman WA et al (2009) Randomized clinical trial of laparoscopic versus open repair of the perforated peptic ulcer: the LAMA Trial. World J Surg 33:1368–1373. doi:10.1007/s00268-009-0054-y
Siu WT, Leong HT, Law BK et al (2002) Laparoscopic repair for perforated peptic ulcer: a randomized controlled trial. Ann Surg 235:313–319
Sanabria A, Villegas MI, Morales Uribe CH (2013) Laparoscopic repair for perforated peptic ulcer disease. Cochrane Database Syst Rev 2:CD004778
Siu WT, Leong HT, Li MK (1997) Single stitch laparoscopic omental patch repair of perforated peptic ulcer. J R Coll Surg Edinb 42:92–94
Agresta F, Ansaloni L, Baiocchi GL et al (2012) Laparoscopic approach to acute abdomen from the Consensus Development Conference of the Società Italiana di Chirurgia Endoscopica e nuove tecnologie (SICE), Associazione Chirurghi Ospedalieri Italiani (ACOI), Società Italiana di Chirurgia (SIC), Società Italiana di Chirurgia d’Urgenza e del Trauma (SICUT), Società Italiana di Chirurgia nell’Ospedalità Privata (SICOP), and the European Association for Endoscopic Surgery (EAES). Surg Endosc 26:2134–2164
Katkhouda N, Mavor E, Mason RJ, Campos GM, Soroushyari A, Berne TV (1999) Laparoscopic repair of perforated duodenal ulcers: outcome and efficacy in 30 consecutive patients. Arch Surg 134:845–848
Lunevicius R, Morkevicius M (2005) Comparison of laparoscopic versus open repair for perforated duodenal ulcers. Surg Endosc 19:1565–1571
Bertleff MJ, Lange JF (2010) Laparoscopic correction of perforated peptic ulcer: first choice? A review of literature. Surg Endosc. 24:1231–1239
Kuwabara K, Matsuda S, Fushimi K, Ishikawa KB, Horiguchi H, Fujimori K (2011) Community-based evaluation of laparoscopic versus open simple closure of perforated peptic ulcers. World J Surg 35:2485–2492. doi:10.1007/s00268-011-1252-y
Kim JM, Jeong SH, Lee YJ et al (2012) Analysis of risk factors for postoperative morbidity in perforated peptic ulcer. J Gastric Cancer 12:26–35
Boey J, Wong J, Ong GB (1982) A prospective study of operative risk factors in perforated duodenal ulcers. Ann Surg 195:265–269
Møller MH, Adamsen S, Thomsen RW, Møller AM (2010) Preoperative prognostic factors for mortality in peptic ulcer perforation: a systematic review. Scand J Gastroenterol 45:785–805
Møller MH, Engebjerg MC, Adamsen S, Bendix J, Thomsen RW (2012) The peptic ulcer perforation (PULP) score: a predictor of mortality following peptic ulcer perforation. A cohort study. Acta Anaesthesiol Scand 56:655–662
Cheng M, Li WH, Cheung MT (2012) Early outcome after emergency gastrectomy for complicated peptic ulcer disease. Hong Kong Med J 18:291–298
Vashist YK, Yekebas EF, Gebauer F et al (2012) Management of the difficult duodenal stump in penetrating duodenal ulcer disease: a comparative analysis of duodenojejunostomy with “classical” stump closure (Nissen-Bsteh). Langenbecks Arch Surg 397:1243–1249
Acknowledgments
All authors do not have any disclosures to make. AY Teoh had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. This study was not supported by any research Grant.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Teoh, A.Y.B., Chiu, P.W.Y., Kok, A.S.Y. et al. The Selective Use of Laparoscopic Repair is Safe in High-Risk Patients Suffering from Perforated Peptic Ulcer. World J Surg 39, 740–745 (2015). https://doi.org/10.1007/s00268-014-2851-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2851-1