Abstract
Background
The incidence of complicated choledochocystolithiasis is increasing with the aging of society in Japan. We evaluated the utility of our prediction rule modified estimation of physiologic ability and surgical stress (mE-PASS) in predicting postoperative adverse events in patients with choledochocystolithiasis.
Methods
A total of 4,329 patients who underwent elective surgery for choledochocystolithiasis in 44 referral hospitals between April 1987 and April 2007 were analyzed for mE-PASS along with postoperative events. The discrimination power of mE-PASS was assessed by the area under the receiver operating characteristic curve (AUC). The correlation between ordinal and interval variables was quantified by the Spearman rank correlation (ρ). The ratio of observed-to-estimated mortality rates (OE ratio) was used as a metric of surgical quality.
Results
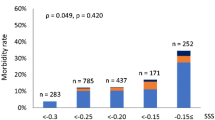
Postoperative in-hospital mortality rates were 0 % (0/3,442) for laparoscopic cholecystectomy, 0.19 % (1/521) for open cholecystectomy, 1.6 % (1/63) for laparoscopic choledochotomy, 1.1 % (3/264) for open choledochotomy, and 5.1 % (2/39) for plasty or resection of the common bile duct. mE-PASS demonstrated a high discrimination power to predict in-hospital mortality; AUC, 95 % confidence interval (CI) of 0.96, 0.94–0.99. The predicted mortality rates significantly correlated with the severity of postoperative complications (ρ = 0.278, p < 0.0001) and length of hospital stay (ρ = 0.479, p < 0.0001). The OE ratios (95 % CI) improved slightly over time; 1.5 (0.25–9.0) between 1987 and 2000, and 0.40 (0.078–2.1) between 2001 and 2007.
Conclusions
The present study suggests that mE-PASS can predict postoperative risks in patients who have undergone choledochocystolithiasis. mE-PASS may be useful in surgical decision making and evaluating the quality of care.


Similar content being viewed by others
References
Kharbutli B, Velanovich V (2008) Management of preoperatively suspected choledocholithiasis: a decision analysis. J Gastrointest Surg 12:1973–1980
Yasuda I (2010) Management of the bile duct stone: current situation in Japan. Dig Endosc 22(Suppl 1):S76–S78
Almadi MA, Barkun JS, Barkun AN (2012) Management of suspected stones in the common bile duct. Can Med Assoc J 184:884–892
Yin Z, Xu K, Sun J et al (2013) Is the end of the T-tube drainage era in laparoscopic choledochotomy for common bile duct stones coming? A systematic review and meta-analysis. Ann Surg 257:54–66
Aiura K, Kitagawa Y (2011) Current status of endoscopic papillary balloon dilation for the treatment of bile duct stones. J Hepatobiliary Pancreat Sci 18:339–345. doi:10.1007/s00534-010-0362-5
Hwang JC, Kim JH, Lim SG et al (2013) Endoscopic large-balloon dilation alone versus endoscopic sphincterotomy plus large-balloon dilation for the treatment of large bile duct stones. BMC Gastroenterol 13:15–20
Teoh AYB, Cheung FKY, Hu B et al (2013) Randomized trial of endoscopic sphincterotomy with balloon dilation versus endoscopic sphincterotomy alone for removal of bile duct stones. Gastroenterology 144:341–345
Haga Y, Ikei S, Ogawa M (1999) Estimation of physiologic ability and surgical stress (E-PASS) as a new prediction scoring system for postoperative morbidity and mortality following elective gastrointestinal surgery. Surg Today 29:219–225
Haga Y, Wada Y, Takeuchi H et al (2004) Estimation of physiological ability and surgical stress (E-PASS) for a surgical audit in elective digestive surgery. Surgery 135:586–594
Haga Y, Ikejiri K, Wada Y et al (2011) A multicenter prospective study of surgical audit systems. Ann Surg 253:194–201
Haga Y, Ikei S, Wada Y et al (2001) Evaluation of an estimation of a physiologic ability and surgical stress (E-PASS) scoring system to predict postoperative risk: a multicenter prospective study. Surg Today 31:569–574
Haga Y, Wada Y, Takeuchi H et al (2002) Estimation of surgical costs using a prediction scoring system estimation of physiologic ability and surgical stress. Arch Surg 137:481–485
Pérez G, Escalona A, Jarufe N et al (2005) Prospective randomized study of T-tube versus biliary stent for common bile duct decompression after open choledochotomy. World J Surg 29:869–872. doi:10.1007/s00268-005-7698-z
Doglietto GB, Gallitelli L, Pacelli F et al (1996) Protein-sparing therapy after major abdominal surgery: lack of clinical effects. Ann Surg 223:357–362
Clavien PA, Barkun J, de Oliveira ML et al (2009) The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Akobeng AK (2007) Understanding diagnostic tests 3: receiver operating characteristic curves. Acta Paediatr 96:644–647
Haga Y, Wada Y, Ikenaga M et al (2011) Evaluation of modified estimation of physiologic ability and surgical stress (mE-PSS) in colorectal carcinoma surgery. Dis Colon Rectum 54:1293–1300
Haga Y, Wada Y, Takeuchi H et al (2012) Evaluation of modified estimation of physiologic ability and surgical stress (mE-PASS) in gastric carcinoma surgery. Gastric Cancer 15:7–14
Haga Y, Ikejiri K, Takeuchi H et al (2012) Value of general surgical risk models for predicting postoperative liver failure and mortality following liver surgery. J Surg Oncol 106:898–904
Yang J, Peng JY, Chen W (2012) Endoscopic biliary stenting for irretrievable common bile duct stones: indications, advantages, disadvantages, and follow-up results. Surgeon 10:211–217
Scollay JM, Mullen R, McPhillips G et al (2011) Mortality associated with the treatment of gallstone disease: a 10-year contemporary national experience. World J Surg 35:643–647. doi:10.1007/s00268-010-0908-3
Miyazaki N, Haga Y, Matsukawa H et al (2013) The development and validation of the calculation of post-operative risk in emergency surgery (CORES) model. Surg Today. doi:10.1007/s00595-013-0707-1
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haga, Y., Wada, Y., Takeuchi, H. et al. Evaluation of Modified Estimation of Physiologic Ability and Surgical Stress in Patients Undergoing Surgery for Choledochocystolithiasis. World J Surg 38, 1177–1183 (2014). https://doi.org/10.1007/s00268-013-2383-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-2383-0