Abstract
Background
A mathematical model for primary hyperparathyroidism (1°HPTH) was developed and embedded in software to yield intraoperative predictability curves.
Methods
A total of 1,754 consecutive 1°HPTH operative cases were screened to select 617 [554 single adenoma (SA), 63 multigland] patients with complete preoperative, intraoperative (pre-exploration, time 0, every 5 min post-resection), and postoperative parathyroid hormone (PTH) and calcium data. Data transformations and models were hypothesized and tested, including inverse functions, differences, half-lives, differences from projected half-lives, second-order kinetics, second-order derivatives, and time-dependent ratios. Sub-models of ratios were developed for time-dependent and initial-value combinations. For each time segment the log odds were modeled using multiple logistic stepwise regression. An idealized model was selected, embedded in software, and installed in a laptop computer to enable intraoperative decision analyses, PTH curve plotting, and storage and transmission of data. A subsequent cohort of 100 consecutive unselected patients [81 SAs, 19 multigland (13 hyperplasia, 2 MEN1, 1 lithium, 3 double adenomas)] inclusive of seven remedial cervical explorations were tested.
Results
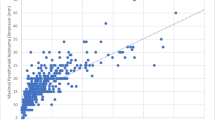
The model predicted an overall curative resection in 95 % of patients. In SA patients, cure was predicted in 78/81 patients with a mean probability of 99.3 % at 11.8 ± 10.4 min post-resection. In three cured patients, the software failed to suggest cure, because of a low baseline PTH or delayed clearance. The model also correctly predicted residual hyperfunctioning tissue in all tested multigland patients. All multigland patients underwent additional exploration with resection of residual disease resulting in a mean predicted cure rate of 97.9 % at 10.6 ± 7.3 min post-resection completion in 17 patients. In two patients, the software predicted a mean cure rate of 22 % due to either a low PTH baseline or delayed clearance. Overall, the software accurately predicted cure in 95 of 100 cured cases.
Conclusions
This intraoperative prediction software expedites termination of surgery with a high level of curative confidence. Alternatively, the model accurately predicts residual disease prompting additional exploration. Because the model is based on a large set of multivariate regression curves, PTH values obtained at any post-resection sampling interval generate prediction data with far greater accuracy than existing algorithms. The software is designed for convenient operative use and can print, store, and electronically transmit probability analyses and PTH curves in real-time.





Similar content being viewed by others
References
Golden SH, Robinson KA, Saldanha I et al (2009) Clinical review: prevalence and incidence of endocrine and metabolic disorders in the United States: a comprehensive review. J Clin Endocrinol Metab 94:1853–1878
Bilezikian JP, Khan AA, Potts JT Jr (2009) Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the Third International Workshop. J Clin Endocrinol Metab 94(2):335–339
Silverberg SJ, Lewiecki EM, Mosekilde L et al (2009) Presentation of Asymptomatic Primary Hyperparathyroidism: Proceedings of the Third International Workshop. J Clin Endocrinol Metab 94(2):351–365
Kunstman JW, Kirsch JD, Mahajan A et al (2013) Parathyroid localization and implications for clinical management. J Clin Endocrinol Metab 98(3):902–912
Starker LF, Fonseca AL, Carling T et al (2011) Minimally invasive parathyroidectomy. Int J Endocrinol 2011:1–8
Sokoll LJ, Donovan P, Udelsman R (2007) The NACB laboratory medicine practice guidelines for intraoperative PTH. Point Care 6:253–260
Udelsman R, Lin Z, Donovan P (2011) The superiority of minimally invasive parathryoidectomy based on 1650 consecutive patients with primary hyperparathyroidism. Ann Surg 253(3):585–591
Carneiro-Pla D (2011) Contemporary and practical uses of intraoperative parathyroid hormone monitoring. Endocr Pract 17(1):44–53
Sokoll LJ, Drew H, Udelsman R (2000) Intraoperative parathyroid hormone analysis: a study of 200 consecutive cases. Clin Chem 46(10):1662–1668
Libutti SK, Alexander HR, Bartlett DL et al (1999) Kinetic analysis of the rapid intraoperative parathyroid hormone assay in patients during operation for hyperparathyroidism. Surgery 126:1145–1151
Riss P, Kaczirek K, Bieglmayer C, Niederle B (2007) PTH spikes during parathyroid exploration—a possible pitfall during PTH monitoring? Langenbecks Arch Surg 392:427–430
Richards MS, Thompson GB, Farley DR, Grant CS (2011) An optimal algorithm for intraoperative parathyroid hormone monitoring. Arch Surg 146(3):280–285
Singh DN, Gupta SK, Chand G et al (2012) Intra-operative parathyroid hormone kinetics and influencing factors with high baseline PTH: a prospective study. Clin Endocrinol 78:935–941
Mazeh H, Chen H, Leverson G, Sippel RS (2013) Creation of a “Wisconsin Index” nomogram to predict the likelihood of additional hypersecreting parathyroid glands during parathyroidectomy. Ann Surg 257:138–141
Davis DD, Tec MC, Kowal J et al (2013) Streamlining of intra-operative parathyroid hormone measurements for cure during parathyroidectomy. Am J Surg 205:597–601
Carneiro DM, Solozano CC, Nader MC et al (2003) Comparison of intraoperative iPTH assay (QPTH) criteria in guiding parathyroidectomy: which criterion is the most accurate? Surgery 134(6):973–979
Acknowledgments
The authors are grateful to Tracy Edwards for assisting with the preparation of this manuscript.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Udelsman, R., Donovan, P. & Shaw, C. Cure Predictability During Parathyroidectomy. World J Surg 38, 525–533 (2014). https://doi.org/10.1007/s00268-013-2327-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-2327-8