Abstract
Background
The purpose of the present study was to describe the impact of treatment of pancreatic and peri-ampullary malignancy on patient reported outcomes (PRO). However, limited data are available describing the impact of curative or palliative therapy on pancreatic/peri-ampullary malignancy and quality of life.
Methods
Patients selected for pancreaticoduodenectomy (PD) completed the European Organisation for Research and Treatment of Cancer QLQ-C30 questionnaire pre-surgery and 6 weeks, 3, 6, 12, 18, and 24 months postoperatively. Patients selected for palliative treatments completed the same questionnaire before treatment and monthly thereafter. Mean scores and 95 % confidence intervals (CI) were calculated for functional scales. Symptom scales and single items were categorized as either minimal or severe, and they were reported as proportions of patients experiencing severe symptoms with 95 % CI.
Results
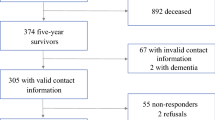
A total of 100 patients (53 planned PD, 47 palliative) were enrolled. Of the 53 patients planned for surgery, 12 had tumors that were unresectable and 41 underwent pancreatoduodenectomy (PD). Seven patients were excluded because of benign histology or concurrent malignancy. Baseline questionnaire compliance was 70 %. For those undergoing PD, there were 53 complications, 7 deaths at 1 year, and 14 deaths at 2 years. Post-surgery most functions and symptoms deteriorated. Recovery in global health and most symptoms occurred by 3 months, and functional scales recovered by 6 months. Recovery of PRO was maintained in the survivors at 2 years. Palliative patients had poorer function and more symptoms at baseline; however, poor follow-up questionnaire compliance prevented further analysis of this group.
Conclusions
Pancreaticoduodenectomy has a short-term negative impact on PRO that recovers within 6 months and is maintained at 2 years in survivors. Further work evaluating palliative and curative treatment in larger patient groups with disease-specific questionnaires is necessary.


Similar content being viewed by others
References
Cancer Research UK (2010) Pancreatic cancer incidence statistics, London, Cancer Research UK
Cascinu S, Falconi M, Valentini V et al (2010) Pancreatic cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 21:v55–v58
Weber A, Mittermeyer T, Wagenpfeil S et al (2009) Self-expanding metal stents versus polyethylene stents for palliative treatment in patients with advanced pancreatic cancer. Pancreas 38:e7–e12
Mossner J (2010) What’s new in therapy of pancreatic cancer? Dig Dis 28:679–683
Moss RA, Lee C (2010) Current and emerging therapies for the treatment of pancreatic cancer. Onco Targets Ther 3:111–127
Neoptolemos JP, Stocken DD, Bassi C et al (2010) Adjuvant chemotherapy with fluorouracil plus folinic acid vs gemcitabine following pancreatic cancer resection. J Am Med Assoc 304:1073–1081
Neoptolemos JP, Stocken DD, Friess H et al (2004) A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N Engl J Med 350:1200–1210
Hernandez JM, Morton CA, Al-Saadi S (2010) The natural history of resected pancreatic cancer without adjuvant chemotherapy. Am Surg 76:480–485
Wilkowski R, Thoma M, Bruns C et al (2006) Combined chemoradiotherapy for isolated local recurrence after primary resection of pancreatic cancer. J Pancreas 7:34–40
Blazeby JM, Avery K, Sprangers M et al (2006) Health-related quality of life measurement in randomized clinical trials in surgical oncology. J Clin Oncol 24:3178–3186
Ohtsuka T, Yamaguchi K, Ohuchida J et al (2003) Comparison of quality of life after pylorus-preserving pancreatoduodenectomy and Whipple resection. Hepatogastroenterology 50:846–850
Huang JJ, Yeo CJ, Sohn TA et al (2000) Quality of life and outcomes after pancreaticoduodenectomy. Ann Surg 231:890–898
Shaw CM, O’Hanlon DM, McEntee GP (2005) Long-term quality of life following pancreaticoduodenectomy. Hepatogastroenterology 52:927–932
Ong HS, Ng EH, Heng G et al (2000) Pancreaticoduodenectomy with pancreaticogastrostomy: assessment of patients’ nutritional status, quality of life and pancreatic exocrine function. Aust N Z J Surg 70:199–203
Kostro J, Sledzinski Z (2008) Quality of life after surgical treatment of pancreatic cancer. Acta Chir Belg 108:679–684
Labori KJ, Hjermstad MJ, Wester T et al (2006) Symptom profiles and palliative care in advanced pancreatic cancer: a prospective study. Support Care Cancer 14:1126–1133
Scheingraber S, Scheingraber T, Brauckhoff M et al (2005) Comparison between a general and a disease-specific health-related quality-of-life questionnaire in patients after pancreatic surgery. J Hepatobiliary Pancreat Surg 12:290–297
Patti MG, Pellegrini CA, Way LW (1987) Gastric emptying and small bowel transit of solid food after pylorus-preserving pancreaticoduodenectomy. Arch Surg 122:528–532
Fink AS, DeSouza LR, Mayer EA et al (1988) Long-term evaluation of pylorus preservation during pancreaticoduodenectomy. World J Surg 12:663–670. doi:10.1007/BF01655880
You YN, Thompson GB, Young WF Jr et al (2007) Pancreatoduodenal surgery in patients with multiple endocrine neoplasia type 1: operative outcomes, long-term function, and quality of life. Surgery 142:829–836 Discussion 836
Witzigmann H, Max D, Uhlmann D et al (2002) Quality of life in chronic pancreatitis: a prospective trial comparing classical Whipple procedure and duodenum-preserving pancreatic head resection. J Gastrointest Surg 6:173–179 Discussion 179–180
Whipple A (1942) Present-day surgery of the pancreas. N Engl J Med 226:515–526
Aaronson NK, Ahmedzai S, Bergman B et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85:365–376
Fayers P, Aaronson N, Bjordal K et al (2002) EORTC QLQ-C30 Scoring Manual. EORTC Publications, Brussels
Osoba D, Rodrigues G, Myles J et al (1998) Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol 16:139–144
Fayers P, Machin D (2007) Quality of life: assessment, analysis and interpretation. John Wiley & Sons, Chichester
Pezzilli R, Falconi M, Zerbi A et al (2011) Clinical and patient-reported outcomes after pancreatoduodenectomy for different diseases: a follow-up study. Pancreas 40:938–945
Chan C, Franssen B, Dominguez I et al (2012) Impact on quality of life after pancreatoduodenectomy: a prospective study comparing preoperative and postoperative scores. J Gastrointest Surg 16:1341–1346
Schwartz CE, Bode R, Repucci N et al (2006) The clinical significance of adaptation to changing health: a meta-analysis of response shift. Qual Life Res 15:1533–1550
Nordin K, Steel J, Hoffman K et al (2001) Alternative methods of interpreting quality of life data in advanced gastrointestinal cancer patients. Br J Cancer 85:1265–1272
Fitzsimmons D, Johnson CD, George S et al (1999) Development of a disease specific quality of life (QoL) questionnaire module to supplement the EORTC core cancer QoL questionnaire, the QLQ-C30 in patients with pancreatic cancer. EORTC Study Group on Quality of Life. Eur J Cancer 35:939–941
National Cancer Institute (2006) The NCI Strategic plan for leading the nation to eliminate the suffering and death due to cancer. US Department of Health and Human Services National Institutes of Health, Washington
ASCO Health Services Research Outcomes Working Group (1996) Outcomes of cancer treatment for technology assessment and cancer treatment guidelines. American Society of Clinical Oncology. J Clin Oncol 96:671–679
Epstein RM, Alper BS, Quill TE (2004) Communicating evidence for participatory decision making. J Am Med Assoc 291:2359–2366
McNair AG, Brookes ST, Davis CR et al (2010) Communicating the results of randomized clinical trials: do patients understand multidimensional patient-reported outcomes? J Clin Oncol 28:738–743
Acknowledgments
This work was funded in part by a personal MRC Clinician Scientist Award (J.M.B.), by the MRC Hub for Trials Methodology Research (ConDuCT) (R.M and J.M.B.), and by the (UK) National Institute of Health Research (J.R. and N.S.B.). The authors are grateful to Joanna Nicklin for collecting the PRO data used in this study and to the members of the Upper Gastrointestinal Multidisciplinary Team at University Hospitals Bristol NHS Foundation Trust.
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
J. R. E. Rees and R. C. Macefield contributed equally to this study.
Rights and permissions
About this article
Cite this article
Rees, J.R.E., Macefield, R.C., Blencowe, N.S. et al. A Prospective Study of Patient Reported Outcomes in Pancreatic and Peri-ampullary Malignancy. World J Surg 37, 2443–2453 (2013). https://doi.org/10.1007/s00268-013-2104-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-2104-8