Abstract
Background
Surgical resection is often recommended in adults with intestinal intussusception (AI) because of its potential association with malignancy. We provide a contemporary algorithm for managing AI by focusing on the probability of discovering a lead point.
Methods
This is a retrospective study of adult patients with computed tomography (CT)-confirmed intussusception who underwent operative management of AI between 1996 and 2011 at a single academic institution.
Results
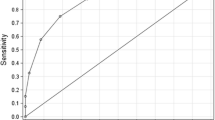
Sixty-four patients were diagnosed with AI by CT scan and then managed operatively. The incidence of colonic (CI), small bowel (SBI), and retrograde intussusception (RI) was 14, 55, and 31 %, respectively. All patients with CI had a lead point, whereas none were found among patients with RI. Some 46 % of patients with SBI had a lead point. The probability of discovering a lead point in SBI was increased by past history of malignancy (RR, 3.7, p < 0.001), a mass seen on preoperative CT scan (RR, 2.9, p = 0.005), and age over 60 years (RR, 2.2, p = 0.07).
Conclusions
A pathologic lead point is likely with CI but not with RI. Patients with SBI who are over the age of 60 years and have a history of malignancy or a mass noted on CT scan have a higher likelihood of harboring a pathologic lead point.
Similar content being viewed by others
References
Agha FP (1986) Intussusception in adults. AJR Am J Roentgenol 146:527–531
Azar T, Berger DL (1997) Adult intussusception. Ann Surg 226:134–138
Barussaud M, Regenet N, Briennon X et al (2006) Clinical spectrum and surgical approach of adult intussusceptions: a multicentric study. Int J Colorectal Dis 21:834–839
Coleman MJ, Hugh TB, May RE et al (1981) Intussusception in the adult. Aust N Z J Surg 51:179–180
Laws HL, Aldrete JS (1976) Small-bowel obstruction: a review of 465 cases. South Med J 69:733–734
Nagorney DM, Sarr MG, McIlrath DC (1981) Surgical management of intussusception in the adult. Ann Surg 193:230–236
Sanders GB, Haga WH, Kinnaird DW (1958) Adult intussusception and carcinoma of the colon. Ann Surg 147:796–804
Lvoff N, Breiman RS, Coakley FV et al (2003) Distinguishing features of self-limiting adult small-bowel intussusception identified at CT. Radiology 227:68–72
Tabrizian P, Nguyen SQ, Greenstein A et al (2010) Significant parameters for surgery in adult intussusception. Surgery 147:227–232
Onkendi EO, Grotz TE, Murray JA et al (2011) Adult intussusception in the last 25 years of modern imaging: is surgery still indicated? J Gastrointest Surg 15:1699–1705
Rea JD, Lockhart ME, Yarbrough DE et al (2007) Approach to management of intussusception in adults: a new paradigm in the computed tomography era. Am Surg 73:1098–1105
Sheth A, Jordan PA (2007) Does small bowel intussusception in adults always require surgery? Dig Dis Sci 52:1764–1766
Sundaram B, Miller CN, Cohan RH et al (2009) Can CT features be used to diagnose surgical adult bowel intussusceptions? AJR Am J Roentgenol 193:471–478
Edwards MA, Grinbaum R, Ellsmere J et al (2006) Intussusception after Roux-en-Y gastric bypass for morbid obesity: case report and literature review of rare complication. Surg Obes Relat Dis 2:483–489
Kasotakis G, Sudan R (2009) Retrograde intussusception after Roux-en-Y gastric bypass for morbid obesity. Obes Surg 19:381–384
Simper SC, Erzinger JM, McKinlay RD et al (2008) Retrograde (reverse) jejunal intussusception might not be such a rare problem: a single group’s experience of 23 cases. Surg Obes Relat Dis 4:77–83
Varban O, Azagury D, Ardestani A et al. (2012) Resection or reduction? The dilemma of managing retrograde intussusception after Roux-en-Y gastric bypass. Surg Obes Relat Dis doi: 10.1016/j.soard.2010.07.015
Begos DG, Sandor A, Modlin IM (1997) The diagnosis and management of adult intussusception. Am J Surg 173:88–94
Eisen LK, Cunningham JD, Aufses AHJ (1999) Intussusception in adults: institutional review. J Am Coll Surg 188:390–395
Wang N, Cui XY, Liu Y et al (2009) Adult intussusception: a retrospective review of 41 cases. World J Gastroenterol 15:3303–3308
Catalano O (1997) Transient small bowel intussusception: CT findings in adults. Br J Radiol 70:805–808
Gupta RK, Agrawal CS, Yadav R et al (2011) Intussusception in adults: institutional review. Int J Surg 9:91–95
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Varban, O.A., Ardestani, A., Azagury, D.E. et al. Contemporary Management of Adult Intussusception: Who Needs a Resection?. World J Surg 37, 1872–1877 (2013). https://doi.org/10.1007/s00268-013-2036-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-2036-3