Abstract
Background
Abdominal tuberculosis (ATB) poses a significant diagnostic, management, and resource challenge. In Australia, an increasing number of tuberculosis (TB) cases are being reported, and we describe our experience of ATB in an Australian tertiary institution.
Methods
All diagnosed cases of tuberculosis (TB) at the Royal North Shore tertiary hospital campus of the University of Sydney are entered prospectively into a central registry. Cases of ATB encountered between September 1991 and November 2011 were identified and retrospectively reviewed.
Results
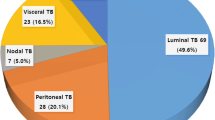
In all, 841 cases of TB were identified, of which 20 were abdominal (2.4 %). Median age at presentation was 34 years (range: 22–79 years), and 55 % of patients were women. None of the patients were born in Australia and 11 patients were of South Asian origin. The most common presenting symptom was abdominal pain (65 %). Diagnosis was based primarily on histology (90 % sensitivity), and the sensitivity of PCR analysis in this series was low (44 %). Eleven of the patients required laparoscopy or laparotomy. 40 % of cases involved the peritoneum, and disease was also seen in solid organs (liver, spleen, pancreas, adrenal gland) and bowel (esophagus, small bowel, colon).
Conclusions
In our local experience ATB was seen exclusively in the immigrant population. The presentation of ATB varies greatly, necessitating a high index of suspicion within the context of abdominal symptoms in high-risk groups. The role of surgical involvement is indispensable for both diagnosis and management of ATB-related complications. Surgeons should remain mindful of the diagnosis in an age of increasing worldwide incidence.
Similar content being viewed by others
References
World Health Organisation (2011) Global tuberculosis control, WHO Report, Geneva, 3,227 pp
World Health Organization (2007) Improving the diagnosis and treatment of smear-negative pulmonary and extrapulmonary tuberculosis among adults and adolescents. Recommendations for HIV-prevalent and Resource-constrained Settings. WHO Report, Geneva, 24 pp
Rasheed S, Zinicola R, Watson D et al (2007) Intra-abdominal and gastrointestinal tuberculosis. Colorectal Dis 9:773–783
Sharma MP, Bhatia V (2004) Abdominal tuberculosis. Indian J Med Res 120:305–315
Yunaev M, Ling A, Abbas S et al (2011) Abdominal tuberculosis: an easily forgotten diagnosis. A N Z J Surg 81:559–560
Pulimood A, Amarapurkar D, Ghoshal U (2011) Differentiation of Crohn’s disease from intestinal tuberculosis in India in 2010. World J Gastroenterol 17:433–443
Donoghue HD, Hotlon JH (2009) Intestinal tuberculosis. Curr Opin Infect Dis 22:490–496
Ramesh J, Banait GS, Ormerod LP (2008) Abdominal tuberculosis in a district general hospital: a retrospective review of 86 cases. Q J Med 101:189–195
Barry C, Konstantinos A, National tuberculosis Advisory Committee (2009) Tuberculosis notifications in Australia, 2007. Commun Dis Intell 33:304–315
King K, Douglas P, Beath K (2011) Is premigration screening for tuberculosis worthwhile? Med J Aust 195:534–537
Plant A, Krause V, Condon J et al (1995) Aborigines and tuberculosis: why they are at risk. Aust J Public Health 19:487–491
Simpson G, Knight T (1999) Tuberculosis in Far North Queensland, Australia. Int J Tuberc Lung Dis 3:1096–1100
Robertus L, Konstantinos A, Hayman N et al (2011) Tuberculosis in the Australian indigenous population: history, current situation and future challenges. Aust N Z J Publ Health 35:6–9
World Health Organization (2010) Treatment of Tuberculosis Guidelines, 4th edn. World Health Organization, Geneva
Chou CH, Ho MW, Ho CM et al (2010) Abdominal tuberculosis in adults: 10-year experience in a teaching Hhspital in central Taiwan. J Microbiol Immunol Infect 43:395–400
Muneef MA, Memish Z, Mahmoud SA et al (2001) Tuberculosis in the belly: a review of forty-six cases involving the gastrointestinal tract and peritoneum. Scand J Gastroenterol 36:528–532
Marshall JB (1993) Tuberculosis of the gastrointestinal tract and peritoneum. Am J Gastroenterol 88:989–999
Lingenfelser T, Zak J, Marks IN et al (1993) Abdominal tuberculosis: still a potentially lethal disease. Am J Gastroenterol 88:744–750
Balthazar EJ, Gordon R, Hulnick D (1990) Ileocecal tuberculosis: CT and radiographic evaluation. Am J Roentgenol 154:499–503
Barry C, Waring J, Stapledon R, National Tuberculosis Advisory Committee (2012) Tuberculosis notifications in Australia, 2008 and 2009. Commun Dis Intell 36:82–94
Lazarus AA, Thilagar B (2007) Abdominal tuberculosis. Dis Mon 53:32–38
Kosseifi S, Hoskere G, Roy TM et al (2009) Peritoneal tuberculosis: modern peril for an ancient disease. South Med J 102:57–59
Krishnan P, Vayoth SO, Dhar P et al (2008) Laparoscopy in suspected abdominal tuberculosis is useful as an early diagnostic method. A N Z J Surg 78:987–989
Bhargava DK, Shriniwas MD, Chopra P et al (1992) Peritoneal tuberculosis: laparoscopic patterns and its diagnostic accuracy. Am J Gastroenterol 87:109–112
Hossain J, al-Aska AK, al Mofleh I (1992) Laparoscopy in tuberculous peritonitis. J R Soc Med 85:89–91
Ri Menzies, Fitzgerald JM, Mulpeter K (1985) Laparoscopic diagnosis of ascites in Lesotho. Br Med J (Clin Res Ed) 291:473–475
Alvares JF, Devarbhavi H, Makhija P et al (2005) Clinical, colonoscopic and histologic profile of colonic tuberculosis in a tertiary hospital. Endoscopy 37:351–356
Salian NV, Rish JA, Eisenach KD et al (1998) Polymerase chain reaction to detect Mycobacterium tuberculosis in histologic specimens. Am J Respir Crit Care Med 158:1150–1155
Kim KM, Lee A, Choi KY et al (1998) Intestinal tuberculosis: clinicopathological analysis and diagnosis by endoscopic biopsy. Am J Gastroenterol 93:606–609
Chawla K, Gupta S, Mukhopadhyay C et al (2009) PCR for M. tuberculosis in tissue samples. J Infect Develop Countries 3:83–87
Gan HT, Chen YQ, Ouyang Q et al (2002) Differentiation between intestinal tuberculosis and Crohn’s disease in endoscopic biopsy specimens by polymerase chain reaction. Am J Gastroenterol 97:1446–1451
Jin XJ, Kim JM, Kim HK et al (2010) Histopathology and TB PCR kit analysis in differentiating the diagnosis of intestinal tuberculosis and Crohn’s disease. World J Gastroenterol 16:2496–2503
Morse DI (1996) Directly observed therapy for tuberculosis. BMJ 312:719–720
Hong Kong Chest Service/British Medical Research Council (1991) Controlled trial of 2, 4, and 6 months of pyrazinamide in 6-month, three-times-weekly regimens for smear-positive pulmonary tuberculosis, including an assessment of a combined preparation of isoniazid, rifampin and pyrazinamide. Results at 30 months. Am Rev Respir Dis 143:700–706
Uygur-Bayramicli O, Dabak G, Dabak R (2003) A clinical dilemma: abdominal tuberculosis. World J Gastroenterol 9:1098–1101
Khan R, Abid S, Jafri W et al (2006) Diagnostic dilemma of abdominal tuberculosis in non-HIV patients: an ongoing challenge for physicians. World J Gastroenterol 12:6371–6375
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gill, P., Coatsworth, N.R., Gundara, J.S. et al. Tuberculosis: Experience in a Low Endemic Area Australian Tertiary Hospital. World J Surg 37, 984–990 (2013). https://doi.org/10.1007/s00268-013-1935-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-1935-7