Abstract
Background
Posttransplant malignancy is one of the major causes inhibiting long-term graft survival. Gastric adenocarcinoma is the most common malignancy in Korea and occurs more frequently in renal transplant recipients compared to that in Western countries. We aimed to analyze the clinical features of the post-renal-transplant gastric cancer and assess factors that can affect the difference in survival.
Methods
Of the 2,157 recipients who underwent renal transplantation at Asan Medical Center between January 1992 and April 2008, the 13 patients diagnosed with gastric adenocarcinoma after transplantation were retrospectively reviewed. We analyzed the effects of primary disease causing end-stage renal disease, type of donor, type of immunosuppressant, induction therapy, and organ rejection on survival after cancer diagnosis. In addition, we evaluated the need for regular gastric cancer screening after transplantation by analyzing the difference in survival between the patients who were and were not screened on a regular basis.
Results
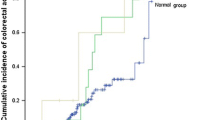
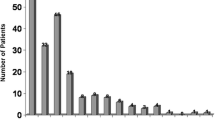
Gastric adenocarcinoma occurred 3.44 times more often in men and 8.33 times more often in women than in the same age group of the general population in Korea (176.4/100,000 in men and 67.6/100,000 in women). Except for endoscopic screening, survival had no relation to the primary disease, type of donor, type of immunosuppressive drug, induction therapy, or the presence of rejection. The 5-year survival rates of recipients who were and were not screened by regular gastroscopic surveillance were 100 and 53.6 %, respectively (p = 0.06).
Conclusions
Regular gastric surveillance might be needed for renal transplant recipients with a high risk of gastric malignancy.

Similar content being viewed by others
References
Meier-Kriesche HU, Schold JD, Srinivas TR et al (2004) Lack of improvement in renal allograft survival despite a marked decrease in acute rejection rates over the most recent era. Am J Transpl 4:378–383
Imao T, Ichimaru N, Takahara S et al (2007) Risk factors for malignancy in Japanese renal transplant recipients. Cancer 109:2109–2115
Andres A (2005) Cancer incidence after immunosuppressive treatment following kidney transplantation. Crit Rev Oncol Hematol 56:71–85
Buell JF, Gross TG, Woodle ES (2005) Malignancy after transplantation. Transplantation 80:S254–S264
Kasiske BL, Snyder JJ, Gilbertson DT et al (2004) Cancer after kidney transplantation in the United States. Am J Transpl 4:905–913
Hoshida Y, Tsukuma H, Yasunaga Y et al (1997) Cancer risk after renal transplantation in Japan. Int J Cancer 71:517–520
Ahn YO, Shin MH (2011) Cancer survival in Seoul, Republic of Korea, 1993–1997. IARC Sci Publ 162:171–178
Persing DH, Prendergast FG (1999) Infection, immunity, and cancer. Arch Pathol Lab Med 123:1015–1022
Selgrad M, Malfertheiner P, Fini L et al (2008) The role of viral and bacterial pathogens in gastrointestinal cancer. J Cell Physiol 216:378–388
Hwang JK, Moon IS, Kim JI (2011) Malignancies after kidney transplantation: a 40-year single-center experience in Korea. Transpl Int 224:716–721
Ju MK, Joo DJ, Kim SJ et al (2009) Chronologically different incidences of post-transplant malignancies in renal transplant recipients: single center experience. Transpl Int 22:644–653
Grulich AE, van Leeuwen MT, Falster MO et al (2007) Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: a meta-analysis. Lancet 370:59–67
Gwack J, Shin A, Kim CS et al (2006) CagA-producing Helicobacter pylori and increased risk of gastric cancer: a nested case-control study in Korea. Br J Cancer 95:639–641
Fock KM, Talley N, Moayyedi P et al (2008) Asia-Pacific consensus guidelines on gastric cancer prevention. J Gastroenterol Hepatol 23:351–365
De Vries AC, Haringsma JK, Kuipers EJ (2007) The detection, surveillance and treatment of premalignant gastric lesions related to Helicobacter pylori infection. Helicobacter 12:1–15
Mera R, Fontham ET, Bravo LE et al (2005) Long term follow up of patients treated for Helicobacter pylori infection. Gut 54:1536–1540
Wong BC, Lam SK, Wong WM et al (2004) Helicobacter pylori eradication to prevent gastric cancer in a high-risk region of China: a randomized controlled trial. JAMA 291:187–194
Dhalla F, da Silva SP, Lucas M et al (2011) Review of gastric cancer risk factors in patients with common variable immunodeficiency disorders, resulting in a proposal for a surveillance programme. Clin Exp Immunol 165:1–7
Conflict of interest
The authors declare no conflict of interest and had no financial support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, IS., Kim, TH., Kim, YH. et al. Clinical Significance of Gastric Cancer Surveillance in Renal Transplant Recipients. World J Surg 36, 1806–1810 (2012). https://doi.org/10.1007/s00268-012-1605-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-012-1605-1