Abstract
Background
Polyacrylamide gel (PAAG) was first manufactured in Ukraine in the late 1980s and introduced as a biomaterial for “breast augmentation without surgery.” Since it is prohibited in most countries, PAAG injections are rare nowadays, but their consequences and long-term complications can be crucial.
Methods
We identified 106 patients consecutively operated on for PAAG complications at three teaching Ukrainian hospitals between 1998 and 2009. All relevant sociodemographic, clinical, and treatment characteristics were collected. Forty-five (42%) patients were available for clinical follow-up.
Results
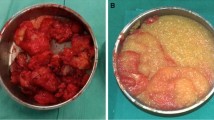
The majority (88%) had had bilateral PAAG injections. The mean volume of injected PAAG was 230 ml/breast (range = 50–400). Mean age at injection was 29 years (range = 17–49) and the mean time from the injection to complications was 6.1 years (SD = 4.1). Symptoms preceding debridement were pain in 85 patients (80%), breast hardening in 79 (74%), breast deformity in 77 (73%), lumps in 57 (54%), gel migration in 39 (37%), fistulas in 17 (16%), and gel leakage in 12 (11%). The surgical interventions in 199 breasts included gel evacuation alone in 107 (54%) or in combination with partial mastectomy in 65 (33%), partial mastectomy and partial pectoralis muscle resection in 12 (6%), or subcutaneous mastectomy in 15 (7%). Of the 199 operated breasts, 86 (43%) immediate and 58 (29%) delayed implant-based breast reconstructions were performed.
Conclusion
Injections of PAAG can cause irreversible damage to the breast necessitating complex debridement procedures, even mastectomy and breast reconstruction. Despite numerous surgical interventions, gel remnants are still found on subsequent breast imaging. Although PAAG is prohibited in many countries, different types of injections with unknown long-term effects are currently being used. Making the public aware of the problems of injectables for breast augmentation is warranted.

Similar content being viewed by others
References
Chasan PE (2007) The history of injectable silicone fluids for soft-tissue augmentation. Plast Reconstr Surg 120:2034–2040, discussion 2041–2033
[No authors listed] (2005) Amended final report on the safety assessment of polyacrylamide and acrylamide residues in cosmetics. Int J Toxicol 24(Suppl 2):21–50
Cheng NX, Zhang YL, Luo SK et al (2011) Late hematoma, seroma, and galactocele in breasts injected with polyacrylamide gel. Aesthet Plast Surg 35:365–372
Cheng NX, Wang YL, Wang JH et al (2002) Complications of breast augmentation with injected hydrophilic polyacrylamide gel. Aesthet Plast Surg 26:375–382
Pallua N, Wolter TP (2010) A 5-year assessment of safety and aesthetic results after facial soft-tissue augmentation with polyacrylamide hydrogel (Aquamid): a prospective multicenter study of 251 patients. Plast Reconstr Surg 125:1797–1804
de Cassia Novaes W, Berg A (2003) Experiences with a new nonbiodegradable hydrogel (Aquamid): a pilot study. Aesthetic Plast Surg 27:376–380
Zarini E, Supino R, Pratesi G et al (2004) Biocompatibility and tissue interactions of a new filler material for medical use. Plast Reconstr Surg 114:934–942
Christensen LH, Breiting VB, Aasted A et al (2003) Long-term effects of polyacrylamide hydrogel on human breast tissue. Plast Reconstr Surg 111:1883–1890
Lemperle G, Rullan PP, Gauthier-Hazan N (2006) Avoiding and treating dermal filler complications. Plast Reconstr Surg 118:92S–107S
Qiao Q, Wang X, Sun J et al (2005) Management for postoperative complications of breast augmentation by injected polyacrylamide hydrogel. Aesthet Plast Surg 29:156–161 (discussion 162)
Luo SK, Chen GP, Sun ZS et al (2011) Our strategy in complication management of augmentation mammaplasty with polyacrylamide hydrogel injection in 235 patients. J Plast Reconstr Aesthet Surg 64(6):731–737
EuroQol Group (1990) EuroQol-a new facility for the measurement of health-related quality of life. Health Policy 16:199–208
Cheung K, Oemar M, Oppe M et al (2009) EQ-5D User Guide. Basic information on how to use EQ-5D: EuroQol Group. http://www.euroqol.org/fileadmin/user_upload/Documenten/PDF/User_Guide_v2_March_2009.pdf. Accessed 24 April 2011
Brandberg Y, Malm M, Rutqvist LE et al (1999) A prospective randomised study (named SVEA) of three methods of delayed breast reconstruction. Study design, patients’ preoperative problems and expectations. Scand J Plast Reconstr Surg Hand Surg 33:209–216
Wewers ME, Lowe NK (1990) A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health 13:227–236
Teo SY, Wang SC (2008) Radiologic features of polyacrylamide gel mammoplasty. AJR Am J Roentgenol 191:W89–W95
Lui CY, Ho CM, Iu PP et al (2008) Evaluation of MRI findings after polyacrylamide gel injection for breast augmentation. AJR Am J Roentgenol 191:677–688
Xu LY, Kong XQ, Tian ZX et al (2006) Magnetic resonance imaging on complications of breast augmentation with injected hydrophilic polyacrylamide gel. Chin Med J (Engl) 119:1311–1314
Lee CJ, Kim SG, Kim L et al (2004) Unfavorable findings following breast augmentation using injected polyacrylamide hydrogel. Plast Reconstr Surg 114:1967–1968
Cheng NX, Xu SL, Deng H et al (2006) Migration of implants: a problem with injectable polyacrylamide gel in aesthetic plastic surgery. Aesthet Plast Surg 30:215–225
Xiao ZB, Liu Y (2008) The relationship between breast cancer and breast augmentation with injected polyacrylamide gel: two case reports. J Plast Reconstr Aesthet Surg 61(8):981–982
Cheng NX, Liu LG, Hui L et al (2009) Breast cancer following augmentation mammaplasty with polyacrylamide hydrogel (PAAG) injection. Aesthet Plast Surg 33:563–569
Abdallah A, Wesemann A, Saklaoui O et al (2009) Breast-conserving treatment of breast cancer after augmentation with injected hydrophilic polyacrylamide gel and review of the literature. Gynakol Geburtshilfliche Rundsch 49:35–38
Golicki D, Niewada M, Jakubczyk M et al (2010) Self-assessed health status in Poland: EQ-5D findings from the Polish valuation study. Pol Arch Med Wewn 120:276–281
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented as an oral presentation at the International Surgical Week (ISW 2011), August 30, 2011, Yokohama, Japan.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Unukovych, D., Khrapach, V., Wickman, M. et al. Polyacrylamide Gel Injections for Breast Augmentation: Management of Complications in 106 Patients, a Multicenter Study. World J Surg 36, 695–701 (2012). https://doi.org/10.1007/s00268-011-1273-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-011-1273-6