Abstract
Background
Pancreatic neuroendocrine tumors (PNETs) are a characteristic feature of the tumor syndromes multiple endocrine neoplasia type 1 (MEN-1) and von Hippel-Lindau disease (VHL). With VHL, about 10% of the patients exhibit PNETs by age 40 years. Metastatic potential is high if the tumors have grown to >3 cm in diameter. Optimal surgical treatment is still a challenge.
Methods
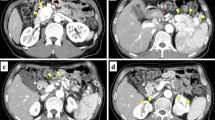
We report three cases, all women, ages 22, 30, and 39 years, respectively, who had known VHL, confirmed by classic organ manifestations and germline mutations of the VHL gene. All were diagnosed, in an asymptomatic stage, with solid tumors of the pancreatic tail or tail/corpus area measuring 2.9–5.6 cm diameter. All accepted the offer of laparoscopic organ-sparing removal of the tumors.
Results
In all three cases, the tumor was entirely removed. In two cases, resection of the spleen was also necessary as dissection of the tumor from the major splenic vessels was impossible. Operating time was 215–365 min, and blood loss was 200–700 ml. Histolopathology revealed benign PNETs in two cases, but the third patient had regional lymph node metastases. There were no complications, and the hospital stay was 4–7 days.
Conclusions
Organ-sparing laparoscopic surgery is an important option for treating VHL-associated PNETs of the pancreatic tail.



Similar content being viewed by others
References
Lonser RR, Glenn GM, Walther M et al (2003) von Hippel-Lindau disease. Lancet 361:2059–2067
Franke G, Bausch B, Hoffmann MM et al (2009) Alu–Alu recombination underlies the vast majority of large VHL germline deletions: molecular characterization and genotype–phenotype correlations in VHL patients. Hum Mutat 30:776–786
Maher ER, Nathanson K, Komminoth P (2004) Von Hippel-Lindau syndrome (VHL). In: DeLellis RA, Lloyd RV, Heitz PU et al (eds) World Health Organization classification of tumours of endocrine organs. IARC Press, Lyon, pp 230–237
Plate KH, Vortmeyer AO, Zagzag D (2007) Von Hippel-Lindau disease and haemangioblastoma. In: Louis DN, Ohgaki H, Wiestler OD et al (eds) WHO classification of tumours of the central nervous system. IARC Press, Lyon, pp 215–217
Corcos O, Couvelard A, Giraud S et al (2008) Endocrine pancreatic tumors in von Hippel-Lindau disease: clinical, histological, and genetic features. Pancreas 37:85–93
Woodward ER, Maher ER (2006) Von Hippel-Lindau disease and endocrine tumour susceptibility. Endocr Relat Cancer 13:415–425
Heitz P, Komminoth P, Perren A et al (2004) Pancreatic endocrine tumours. In: DeLellis RA, Lloyd RV, Heitz PU et al (eds) World Health Organization classification of tumours: pathology and genetics. Tumours of endocrine organs. IARC Press, Lyon, pp 175–182
Libutti SK, Choyke PL, Alexander HR et al (2000) Clinical and genetic analysis of patients with pancreatic neuroendocrine tumors associated with von Hippel-Lindau disease. Surgery 128:1022–1027 discussion 1027–1028
Grubb RL 3rd, Choyke PL, Pinto PA et al (2005) Management of von Hippel-Lindau-associated kidney cancer. Nat Clin Pract Urol 2:248–255
Neumann HP, Eng C (2009) The approach to the patient with paraganglioma. J Clin Endocrinol Metab 94:2677–2683
Kim SC, Park KT, Hwang JW et al (2008) Comparative analysis of clinical outcomes for laparoscopic distal pancreatic resection and open distal pancreatic resection at a single institution. Surg Endosc 22:2261–2268
Langer P, Fendrich V, Bartsch DK (2009) Minimally invasive resection of neuroendocrine pancreatic tumors. Chirurg 80:105–112
Assalia A, Gagner M (2004) Laparoscopic pancreatic surgery for islet cell tumors of the pancreas. World J Surg 28:1239–1247
Fernandez-Cruz L, Blanco L, Cosa R et al (2008) Is laparoscopic resection adequate in patients with neuroendocrine pancreatic tumors? World J Surg 32:904–917
Gagner M, Pomp A (1997) Laparoscopic pancreatic resection: is it worthwhile? J Gastrointest Surg 1:20–25 discussion 25–26
Mabrut JY, Fernandez-Cruz L, Azagra JS et al (2005) Laparoscopic pancreatic resection: results of a multicenter European study of 127 patients. Surgery 137:597–605
Spitz JD, Lilly MC, Tetik C et al (2000) Ultrasound-guided laparoscopic resection of pancreatic islet cell tumors. Surg Laparosc Endosc Percutan Tech 10:168–173
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
von Dücker, L., Walz, M.K., Voss, C. et al. Laparoscopic Organ-Sparing Resection of Von Hippel-Lindau Disease-Associated Pancreatic Neuroendocrine Tumors. World J Surg 35, 563–567 (2011). https://doi.org/10.1007/s00268-010-0878-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-010-0878-5