Abstract
Background
Inflammatory bowel disease (IBD) and colorectal surgery are risk factors for deep venous thrombosis (DVT). The aim of this prospective study was to evaluate the effectiveness of standardized prophylactic low molecular weight heparin (LMWH) therapy in patients who underwent surgery for ulcerative colitis (UC) and Crohn’s disease (CD).
Patients and methods
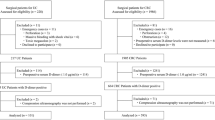
Since 1999 all patients operated on for colorectal diseases in our institute have received 4,000 IU/day LMWH from the day of operation to discharge. The complete series of patients who had major colorectal surgery from 1999 until 2006 were reviewed for overt DVT episodes. Furthermore, 60 consecutive patients who were admitted for surgery for IBD were prospectively enrolled in the 2004–2006 period. Each patient underwent venous color Doppler ultrasound scan at admission and at discharge. Demographic data, disease activity, and clotting parameters were collected. Data were analyzed with Spearman’s correlation test, multiple regression, and receiver operating characteristics (ROC) curves analysis.
Results
The rate of DVT in UC patients was significantly higher than in colorectal cancer patients (p = 0.009), and the odds ratio (OR) for postoperative DVT in UC patients was 7.4 (95% CI 1.4–44.4; p = 0.017). Female gender, UC diagnosis, active rectal bleeding, aPTT value, aCL IgM, aβ2 IgM, and pANCA levels significantly correlated with postoperative DVT. At multivariate analysis only aCL IgM levels were found to be independently associated with postoperative DVT (p = 0.05).
Conclusions
In conclusion, our study showed that prophylactic therapy with 4,000 IU/day LMWH was not completely effective for the prevention of postoperative DVT in patients with CD, and even less so in those with UC. In these patients, a more tailored prophylactic therapy should be considered, and further randomized controlled trials testing the effectiveness of different prophylactic protocols would be advisable. Furthermore, aCL IgM serum levels might be helpful in identifying IBD patients who are at higher risk of postoperative DVT.

Similar content being viewed by others
References
Bargen JA, Barker NW (1936) Extensive arterial and venous thrombosis complicating chronic ulcerative colitis. Arch Intern Med 58:17–31
Nguyen GC, Sam J (2008) Rising prevalence of venous thromboembolism and its impact on mortality among hospitalized inflammatory bowel disease patients. Am J Gastroenterol 103:2272–2280
Miehsler W, Reinisch W, Valic E et al (2003) Is inflammatory bowel disease an independent and disease specific risk factor for thromboembolism? Gut 53:542–548
Van Bodegraven AA, Schoorl M, Baak JPA et al (2001) Haemostatic imbalance in active and quiescent ulcerative colitis. Am J Gastroenterol 96:487–493
Solem CA, Loftus EY, Tremaine WJ et al (2003) Venous thromboembolism in inflammatory bowel disease. Am J Gastroenterol 98:97–101
Larsen TB, Nielsen JN, Freholm L et al (2002) Hyperhomocysteinaemia, coagulation pathway activation and thrombophilia in patients with inflammatory bowel disease. Scand J Gastroenterol 1:62–67
Saibeni S, Bottasso B, Spina L et al (2004) Assessment of thrombin-activable fibrinolysis inhibitor plasma levels in inflammatory bowel diseases. Am J Gastroenterol 99:1966–1970
Novacek G, Miehsler W, Kapiotis S et al (1999) Thromboembolism and resistance to activated protein C in patients with inflammatory bowel disease. Am J Gastroenterol 94:685–690
Saibeni S, Cattaneo M, Vecchi M et al (2003) Low vitamin B6 plasma levels, a risk factor for thrombosis, in inflammatory bowel disease: role of inflammation and correlation with acute phase reactants. Am J Gastroenterol 98:112–117
Romagnuolo J, Fedorak RN, Dias VC et al (2001) Hyperhomocysteineimia and inflammatory bowel disease: prevalence and predictors in a cross sectional study. Am J Gastroenterol 96:2143–2149
Quera R, Shanahan F (2004) Thromboembolism: an important manifestation of inflammatory bowel disease. Am J Gastroenterol 99:1971–1973
Borly L, Wille-Jorgesen P, Rasmussen MS (2005) Systematic review of thromboprohylaxis in colorectal surgery-an update. Colorectal Dis 7:122–127
Lee FY, Hu R, Leung YF et al (2001) Incidence of deep vein thrombosis after colorectal surgery in a Chinese population. ANZ J Surg 71:637–640
Ramirez JI, Vassliu P, Gonzalez-Ruiz C et al (2003) Sequential compression devices as prophylaxis for venous thromboembooism in high-risk colorectal patients: reconsidering American Society of Colorectal Surgeons parameters. Am Surg 69:941–945
Catheline JM, Turner R, Gaillard JL et al (1999) Thormboembolism in laparoscopic surgery: risk factors and preventive measures. Surg Laparosc Endosc Percutan Tech 9:135–139
Wille-Jorgesen P, Rasmussen MS, Andersen BR et al (2003) Heparins and mechanical methods for thromboprophylaxis in colorectal surgery. Cochrane Database Syst Rev (4):CD001217
McLeod RS, Wh Geerts, Sniderman KW et al (2001) Subcutaneus heparin versus mow molecular weight heparin as thromboprophylaxis in patients underrgoing colorctal surgery: results of the Canadian colorectal DVT prophylaxis randomized trial. Ann Surg 233:430–444
Harvey RF, Bradshaw JM (1980) A simple index of Crohn’s disease activity. Lancet 1:514
Kane SV, Sandborn WJ, Rufo PA et al (2003) Fecal lactoferrin is a sensitive and specific marker in identifying intestinal inflammation. Am J Gastroenterol 98:1309–1314
Pengo V, Biasiolo A, Fior MG (1995) Autoimmune antiphospholipid antibodies are directed against a cryptic epitope expressed when b2-glycoprotein-I is bound to a suitable surface. Thromb Haemost 73:29
Pengo V, Biasiolo A, Brocco T et al (1996) Autoantibodies to phospholipid binding plasma proteins in patients with thrombosis and phospholipid–reactive antibodies. Thromb Haemost 75:721
Ruffolo C, Scarpa M, Faggian D et al (2007) Cytokine network in chronic perianal Crohn’s disease and indeterminate colitis after colectomy. J Gastrointest Surg 11:16–21
Henderson AR (1993) Assessing test accurancy on its clinical consequence: a primer for receiver operating characteristics curve analysis. Ann Clin Biochem 30:521–539
Endler G, Marsik C, Jilma B et al (2006) Anti-cardiolipin antibodies and overall survival in a large cohort: preliminary report. Clin Chem 52:1040–1044
Marai I, Shechter M, Langevitz P et al (2008) Anti-cardiolipin antibodies and endothelial function in patients with coronary artery disease. Am J Cardiol 101:1094–1097
Locht H, Wiik A (2006) IgG and IgM isotypes of anti-cardiolipin and anti-beta2-glycoprotein I antibodies reflect different forms of recent thrombo-embolic events. Clin Rheumatol 25:246–250
Remková A, Kovácová E, Príkazská M et al (2000) Thrombomodulin as a marker of endothelium damage in some clinical conditions. Eur J Intern Med 11:79–84
Acknowledgments
The authors are grateful to Raffaella Marin and Silvia Zannoni (Clinica Medica I, University of Padova, Italy) for assistance in preserving serum samples. Teresa Filosa, Matteo Bertin, and Silvia Basato (Clinica Chirurgica I, University of Padova, Italy) who retrieved the patient histories, are also gratefully acknowledged. This work was funded, in part, by the MIUR grant ex 60%.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Scarpa, M., Pilon, F., Pengo, V. et al. Deep Venous Thrombosis After Surgery for Inflammatory Bowel Disease: Is Standard Dose Low Molecular Weight Heparin Prophylaxis Enough?. World J Surg 34, 1629–1636 (2010). https://doi.org/10.1007/s00268-010-0490-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-010-0490-8