Abstract
Background
Glycemic control of type 2 diabetes mellitus (T2DM) remains a dilemma to physicians. Although gastric bypass surgery undertaken for morbid obesity has been shown to resolve this disease well, data on the effectiveness of duodenojejunal bypass in improving or resolving T2DM and the metabolic syndrome (MS), especially in nonobese patients are scarce. This study was intended to evaluate the clinical effects of laparoscopic duodenojejunal bypass (LDJB) in patients with T2DM and a body mass index of <35 kg/m2.
Methods
We conducted a 12-month prospective study on the changes in glucose homeostasis and the MS in seven T2DM subjects undergoing LDJB with similar DM duration, type of DM treatment, and glycemic control. Laboratory values including glycosylated hemoglobin A (HbA1c), fasting blood glucose, cholesterol, triglyceride, and C-peptide were followed throughout the 12 months. Serum levels of gastric inhibitory peptide and ghrelin were followed for 1 month. Serum levels of gastrin and glucagon-like peptide were followed for 3 months.
Results
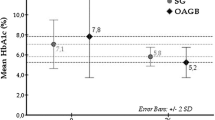
At 12 months after surgery, all subjects consistently felt relief from fatigue, pain and/or numbness in the extremities, polyuria, and polydypsia. Clinical resolution was obtained for one patient, and the preoperative diabetic medication requirements decreased for most of the other patients. The subjects demonstrated an overall improved HbA1c (from 9.4% to 8.5%) and fasting blood glucose level (from 209 to 154 mg/dl). Although the change in fasting blood glucose approached statistical significance, these measures of glucose homeostasis did not achieve significance. Cholesterol and triglycerides increased slightly, and C-peptide decreased slightly over 1 year. These changes were not statistically significant.
Conclusions
Although this is a small series, our data show that at 12 months after surgery, clinical improvement was obvious in all of our seven patients, but LDJB may not be effective at inducing remission of T2DM and the MS in certain patients undergoing this operation. This suggests that larger patient studies should be conducted, before concluding that surgery may offer clinical and biochemical resolution to a disease once treated only medically. Longer follow-up is required for better evaluation.

Similar content being viewed by others
References
King H, Aubert RE, Herman WH (1998) Global burden of diabetes, 1995–2025: prevalence, numerical estimates, and projections. Diabetes Care 21:1414–1431
Narayan KM, Gregg EW, Fagot-Campagna A et al (2000) Diabetes—a common, growing, serious, costly, and potentially preventable public health problem. Diabetes Res Clin Pract 50(Suppl 2):S77–S84
Centers for Disease Control website. www.CDC.com
Harris MI (1995) Summary. In: National diabetes data group (ed) Diabetes in America. NIH publ. 95-1468, 2nd edn. Government Printing Office, Washington, DC, pp 1–14
International Diabetes Federation Task Force on Diabetes Health Economics (1997) Diabetes health economics: facts, figures, and forecasts. International Diabetes Federation, Brussels
Rubino F, Gagner M (2002) Potential of surgery for curing type 2 diabetes mellitus. Ann Surg 236:554–559
Buchwald H, Avidor Y, Braunwald E et al (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292:1724–1737
Ackerman NB (1990) Physiologic approaches to the control of obesity [letter; comment]. Ann Surg 211:107
Pories WJ, Swanson MS, MacDonald KG et al (1995) Who would have thought it? an operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg 222:339–352
Pories WJ, Albrecht RJ (2001) Etiology of type II diabetes mellitus: role of the foregut. World J Surg 25:527–531
De Paula AL, Macedo AL, Prudente AS et al (2006) Laparoscopic sleeve gastrectomy with ileal interposition (“neuroendocrine brake”): pilot study of a new operation. Surg Obes Relat Dis 2:464–467
Vidal J, Ibarzabal A, Romero F et al (2008) Type 2 diabetes mellitus and the metabolic syndrome following sleeve gastrectomy in severely obese subjects. Obes Surg 18:1077–1082
Rubino F, Marescaux J (2004) Effect of duodenal exclusion in a non-obese animal model of type 2 diabetes: a new perspective for an old disease. Ann Surg 239:1–11
Cohen RV, Schiavon CA, Pinheiro JS et al (2007) Duodenal-jejunal bypass for the treatment of type 2 diabetes in patients with body mass index 22–34 kg/m2: a report of 2 cases. Surg Obes Relat Dis 3:195–197
Cohen RV (2007) Duodenojejunal bypass for the treatment of type II diabestes mellitus in patients with BMI 22-34. Presented at the center for the surgical treatment of morbid obesity and metabolic disorders, Hospital Sao Camilo and Baros Surgical Associates, Sao Paulo, Brazil
Schauer PR, Burguera B, Ikramuddin S et al (2003) Effect of laparoscopic Roux-en-Y gastric bypass on type 2 diabetes mellitus. Ann Surg 238:467–484
Torquati A, Lutfi R, Abumrad N et al (2005) Is Roux-en-Y gastric bypass surgery the most effective treatment for type 2 diabetes mellitus in morbidly obese patients? J Gastrointest Surg 9:1112–1118
Dixon JB, O’Brien PE, Playfair J et al (2008) Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial. JAMA 299:316–323
ACCORD trial protocol. Accessed at www.ACCORD.org
Acknowledgments
We thank Kell Julliard for his assistance with the statistical calculations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ferzli, G.S., Dominique, E., Ciaglia, M. et al. Clinical Improvement After Duodenojejunal Bypass for Nonobese Type 2 Diabetes Despite Minimal Improvement in Glycemic Homeostasis. World J Surg 33, 972–979 (2009). https://doi.org/10.1007/s00268-009-9968-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-009-9968-7