Abstract
Introduction
This study was designed to look at the conversion rates and morbidity associated with laparoscopic operations performed by trainee surgeons ascending the learning curve when they are well supervised by staff surgeons.
Methods
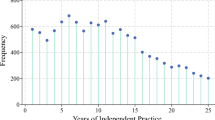
A review of 204 consecutive cases was performed. We defined experienced staff surgeons as those who have performed more than 300 laparoscopic resection cases. The trainee surgeons had less than 50 cases of experience during the study period. All operations were performed by the experienced staff surgeon or by the trainee surgeon with the staff surgeon as the first assistant and supervisor.
Results
A total of 204 laparoscopic resections for colorectal cancer were studied. The dissection was D3 in 73% (n = 149) of cases with a mean lymph node harvest of 19.4 nodes (range 1–56). The staff surgeons performed 90 cases and trainees performed 114 cases. Twenty-one cases (10.3%) required conversion. The overall morbidity rate was 17.6% and perioperative mortality rate was 1.5%. On bivariate analysis, trainee surgeons were not found to be significantly associated with a higher conversion risk. Multivariate analysis revealed that only the factor of T3 and above was an independent predictor of conversion (odds ratio (OR) 4.1; 95% confidence interval (CI) 1.09–15.48). Multivariate analysis of risk factors for morbidity revealed that it was not conversion (OR 2.37; 95% CI, 0.86–6.76) but rectal surgery (OR 4.09; 95% CI 2.04–9.9) that was the independent risk factor of morbidity.
Conclusions
Inexperienced surgeons do not cause more conversions or postoperative morbidity in laparoscopic colorectal surgery if they are well supervised. Conversion is not independently associated with increased postoperative morbidity.
Similar content being viewed by others
References
Jacobs M, Verdeja JC, Goldstein HS (1991) Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc 1:144–150
Sekimoto M (2007) Laparoscopic resection for colorectal cancer in Japan. Dis Colon Rectum 50:1708–1714
Konishi F, Okada M, Nagai H et al (1996) Laparoscopic-assisted colectomy with lymph node dissection for invasive carcinoma of the colon. Surg Today 26:882–889
Finlayson E, Nelson H (2005) Predicting quality in surgery. Br J Surg 92:129–130
Larson DW, Marcello PW, Larach SW et al (2008) Surgeon volume does not predict outcomes in the setting of technical credentialing: results from a randomized trial in colon cancer. Ann Surg 248:746–750
Schlachta CM, Mamazza J, Seshadri PA et al (2001) Defining a learning curve for laparoscopic colorectal resections. Dis Colon Rectum 44:217–222
Reissman P, Cohen S, Weiss EG, Wexner SD (1996) Laparoscopic colorectal surgery: ascending the learning curve. World J Surg 20:277–282
CR JSC (2009) Japanese classification of colorectal carcinoma by Japanese Society for Cancer of the Colon and Rectum. Kanehara & Co Ltd., Tokyo
Tekkis PP, Senagore AJ, Delaney CP (2005) Conversion rates in laparoscopic colorectal surgery: a predictive model with, 1253 patients. Surg Endosc 19:47–54
Abraham NS, Byrne CM, Young JM, Solomon MJ (2007) Meta-analysis of non-randomized comparative studies of the short-term outcomes of laparoscopic resection for colorectal cancer. ANZ J Surg 77:508–516
Gonzalez R, Smith CD, Mason E et al (2006) Consequences of conversion in laparoscopic colorectal surgery. Dis Colon Rectum 49:197–204
Guillou PJ, Quirke P, Thorpe H et al (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365(9472):1718–1726
Tjandra JJ, Chan MK (2006) Systematic review on the short-term outcome of laparoscopic resection for colon and rectosigmoid cancer. Colorectal Dis 8:375–388
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242:83–91
Schlachta CM, Mamazza J, Seshadri PA et al (2000) Predicting conversion to open surgery in laparoscopic colorectal resections. A simple clinical model. Surg Endosc 14:1114–1117
Thorpe H, Jayne DG, Guillou PJ et al (2008) Patient factors influencing conversion from laparoscopically assisted to open surgery for colorectal cancer. Br J Surg 95:199–205
Rotholtz NA, Laporte M, Zanoni G et al (2008) Predictive factors for conversion in laparoscopic colorectal surgery. Tech Coloproctol 12:27–31
Yamamoto S, Yoshimura K, Konishi F, Watanabe M (2008) Phase II trial to evaluate laparoscopic surgery for Stage 0/I rectal carcinoma. Jpn J Clin Oncol 38:497–500
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maeda, T., Tan, KY., Konishi, F. et al. Trainee Surgeons Do Not Cause More Conversions in Laparoscopic Colorectal Surgery if They Are Well Supervised. World J Surg 33, 2439–2443 (2009). https://doi.org/10.1007/s00268-009-0188-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-009-0188-y