Abstract
Background
The aim of this study was to determine the prevalence of hypothyroidism in patients with benign breast disorders (BBD). We then asked if thyroxine replacement in hypothyroid patients has any impact on the clinical outcome of the BBD.
Methods
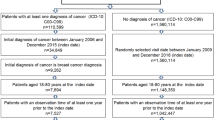
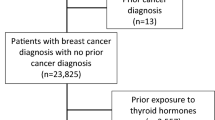
This prospective study included 201 women with BBD. None of the included patients had previously suspected hypothyroidism. Clinical, laboratory, and follow-up details of the patients were noted. Baseline serum thyroxine, thyroid-stimulating hormone (TSH), and prolactin estimation was done in all cases. Thyroid peroxidase antibody (TPOAb) estimation was done in hypothyroid patients and/or patients with a goiter. In addition to the standard conservative management protocol, hypothyroid patients were given thyroxine replacement therapy. Their response to treatment was assessed at 3-month intervals. The clinical outcomes of euthyroid and hypothyroid groups were compared.
Results
The mean age of the patients was 34 ± 8 years, and the mean length of follow-up was 13.0 ± 4.2 months. The overall prevalence of hypothyroidism was 23.2% (nipple discharge 37%, mastalgia 23%, lump/lumpiness 17.4%). The rate of hypothyroidism and the mean serum TSH concentration were significantly higher among patients with nipple discharge than among those with mastalgia (P = 0.001) or a lump (P = 0.01). In all, 39% of hypothyroid women had TSH concentrations >10 mIU/l, and 53% had an elevated TPOAb titer. BBD symptoms were alleviated in 83% of the hypothyroid patients with only thyroxine replacement. The final clinical outcomes of hypothyroid patients with nipple discharge and mastalgia were significantly better than that of their euthyroid counterparts (P = 0.028 and 0.001, respectively); no significant difference was noted in patients with lumpiness (P = 0.144).
Conclusions
All women with BBD should be screened for hypothyroidism because the prevalence of hypothyroidism is high among this group and correction of hypothyroidism results in significant clinical improvement of BBD in most of these patients.



Similar content being viewed by others

References
Barton MB, Elmore JG, Fletcher SW (1999) Breast symptoms among women enrolled in a health maintenance organization: frequency, evaluation, and outcome. Ann Intern Med 130:651–657
Dawson C, Armstrong MW, Michaels J et al (1993) Breast disease and the general surgeon. II. Effect of audit on the referral of patients with breast problems. Ann R Coll Surg Engl 75:83–86
Goehring C, Morabia A (1997) Epidemiology of benign breast disease, with special attention to histologic types. Epidemiol Rev 19:310–327
Peters F, Schuth W, Scheurich B et al (1984) Serum prolactin levels in patients with fibrocystic breast disease. Obstet Gynecol 64:381–385
Watt-Boolsen S, Eskildsen PC, Blaehr H (1985) Release of prolactin, thyrotropin, and growth hormone in women with cyclical mastalgia and fibrocystic disease of the breast. Cancer 56:500–502
Minton JP, Abou-Issa H (1989) Nonendocrine theories of the etiology of benign breast disease. World J Surg 13:680–684
Adamopoulos DA, Vassilaros S, Kapolla N et al (1986) Thyroid disease in patients with benign and malignant mastopathy. Cancer 57:125–128
Giustarini E, Pinchera A, Fierabracci P et al (2006) Thyroid autoimmunity in patients with malignant and benign breast diseases before surgery. Eur J Endocrinol 154:645–649
Venturi S (2001) Is there a role for iodine in breast diseases? Breast 10:379–382
Ghent WR, Eskin BA, Low DA et al (1993) Iodine replacement in fibrocystic disease of the breast. Can J Surg 36:453–460
Estes NC (1981) Mastodynia due to fibrocystic disease of the breast controlled with thyroid hormone. Am J Surg 42:764–766
Goodson WH, Moore DH (2002) Overall clinical breast examination as a factor in delayed diagnosis of breast cancer. Arch Surg 137:1152–1156
Surks MI, Ortiz E, Daniels GH et al (2004) Subclinical thyroid disease: scientific review and guidelines for diagnosis and management. JAMA 291:228–238
Mansel RE, Fenn NJ, Davies EL (1998) Benign breast disease and its management. In: Johnson CD, Taylor I (eds) Recent advances in surgery, vol 21. Churchill Livingstone, Edinburgh, pp 71–83
Delange F, Bastiani S, Benmiloud M (1986) Definitions of endemic goiter and cretinism, classification of goiter size and the severity of endemias, and survey techniques. In: Dunn JT, Pretell EA, Daza CH et al (eds) Towards the eradication of endemic goiter, cretinism, and iodine deficiency. Pan American Health Organization, Washington, DC, p 502
Saraiva PP, Figueiredo NB, Padovani CR et al (2005) Profile of thyroid hormones in breast cancer patients. Braz J Med Biol Res 38:761–765
Shering SG, Zbar AP, Moriarty M et al (1996) Thyroid disorders and breast cancer. Eur J Cancer Prev 5:504–506
Cristofanilli M, Yamamura Y, Kau SW et al (2005) Thyroid hormone and breast carcinoma: primary hypothyroidism is associated with a reduced incidence of primary breast carcinoma. Cancer 103:1122–1128
Rao VR, Lakshmi A, Sadhnani MD (2008) Prevalence of hypothyroidism in recurrent pregnancy loss in first trimester. Indian J Med Sci 62:359–363
Gupta S, Saha PK, Mukhopadhyay A (2008) Prevalence of hypothyroidism and importance of cholesterol estimation in patients suffering from major depressive disorder. J Indian Med Assoc 106:240–242
Baloch Z, Carayon P, Conte-Devolx B et al (2003) Guidelines committee, national academy of clinical biochemistry: laboratory medicine practice guidelines—laboratory support for the diagnosis and monitoring of thyroid disease. Thyroid 13:3–126
Baskin HJ, Cobin RH, Duick DS et al (2002) American Association of Clinical Endocrinologists medical guidelines for clinical practice for the evaluation and treatment of hyperthyroidism and hypothyroidism. Endocr Pract 8:457–469
Vanderpump MP, Tunbridge WH, French JM (1995) The incidence of thyroid disorders in the community: a twenty-year follow-up of the Whickham survey. Clin Endocrinol (Oxf) 43:55–68
Wilson GR, Curry RW (2005) Subclinical thyroid disease. Am Fam Physician 72:1517–1524
Arrigo T, Wasniewska M, Crisafulli G et al (2008) Subclinical hypothyroidism: the state of the art. J Endocrinol Invest 31:79–84
Author information
Authors and Affiliations
Corresponding author
Additional information
P. R. K. Bhargav and A. Mishra have equally contributed to this study.
Rights and permissions
About this article
Cite this article
Bhargav, P.R.K., Mishra, A., Agarwal, G. et al. Prevalence of Hypothyroidism in Benign Breast Disorders and Effect of Thyroxine Replacement on the Clinical Outcome. World J Surg 33, 2087–2093 (2009). https://doi.org/10.1007/s00268-009-0143-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-009-0143-y