Abstract
Background
Outcomes of immediate breast reconstructions can be influenced by postoperative radiotherapy. However, there is no clarity on the use of prepectoral or subpectoral breast reconstruction in the setting of postmastectomy radiation therapy (PMRT). We reviewed evidence on the complication rates of prepectoral and subpectoral breast reconstruction in women undergoing PMRT.
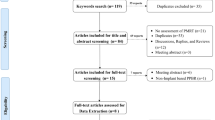
Methods
PubMed, Web of Science, and Embase databases were scanned for studies comparing complication rates of prepectoral and subpectoral breast reconstruction with PMRT. All complications were pooled in a random-effect meta-analysis to obtain odds ratio (OR).
Results
Eight observational studies were included. Meta-analysis showed no difference in the risk of infections (OR: 1.22 95% CI 0.79, 1.88 I2=0%), implant loss (OR: 0.86 95% CI 0.50, 1.50 I2=14%), seroma (OR: 1.01 95% CI 0.43, 2.34 I2=50%), hematoma (OR: 0.44 95% CI 0.12, 1.71 I2=0%), wound dehiscence (OR: 0.95 95% CI 0.42, 2.17 I2=0%), and skin necrosis (OR: 0.61 95% CI 0.21, 1.75 I2=36%), contracture (OR: 0.46 95% CI 0.15, 1.48 I2=54%) and the need for revision surgeries (OR: 0.85 95% CI 0.45, 1.60 I2=15%) between the prepectoral and subpectoral groups.
Conclusions
Data from observational studies indicates that in appropriately selected patients there may not be any difference in the risk of early complications with prepectoral or subpectoral breast reconstruction with PMRT. Current evidence is limited by the small number of studies, short follow-up and selection bias. There is a need for randomized controlled trials comparing the two approaches to obtain robust evidence on long-term outcomes.
Level of Evidence III
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to Table of Contents or the online Instructions to Authors www.springer.com/00266.









Similar content being viewed by others
References
Li JG, Zhao AX, Tan ZQ et al (2023) Effects of different targeted therapies associated with adjuvant chemotherapy on clinical remission, survival and safety in patients with triple-negative breast cancer: a systematic review and meta-analysis. Eur Rev Med Pharmacol Sci 27:7768–7780. https://doi.org/10.26355/eurrev_202308_33431
Agrawal A (2019) Oncoplastic breast surgery and radiotherapy-adverse aesthetic outcomes, proposed classification of aesthetic components, and causality attribution. Breast J 25:207–218. https://doi.org/10.1111/tbj.13193
Zhang C, Hu G, Biskup E et al (2018) Depression induced by total mastectomy, breast conserving surgery and breast reconstruction: a systematic review and meta-analysis. World J Surg 42:2076–2085. https://doi.org/10.1007/s00268-018-4477-1
Song Y, Sun S, Li D et al (2021) Long-term oncologic safety of immediate reconstructive surgery in patients with invasive breast cancer: a retrospective matched-cohort study. World J Surg Oncol 19:348. https://doi.org/10.1186/s12957-021-02450-9
Yoon AP, Qi J, Brown DL et al (2018) Outcomes of immediate versus delayed breast reconstruction: results of a multicenter prospective study. Breast 37:72–79. https://doi.org/10.1016/j.breast.2017.10.009
Sekiguchi K, Kawamori J, Yamauchi H (2017) Breast reconstruction and postmastectomy radiotherapy: complications by type and timing and other problems in radiation oncology. Breast Cancer 24:511–520. https://doi.org/10.1007/s12282-017-0754-3
Zeng L, Xie X-Q, Luo T et al (2021) Progress of radiotherapy after breast-conserving surgery combined with silicone prosthesis reconstruction. Eur Rev Med Pharmacol Sci 25:2193–2198. https://doi.org/10.26355/eurrev_202103_25210
Caputo GG, Zingaretti N, Kiprianidis I et al (2021) Quality of life and early functional evaluation in direct-to-implant breast reconstruction after mastectomy: a comparative study between prepectoral versus dual-plane reconstruction. Clin Breast Cancer 21:344–351. https://doi.org/10.1016/j.clbc.2020.11.013
Lo Torto F, Marcasciano M, Kaciulyte J et al (2020) Prepectoral breast reconstruction with TiLoop® Bra Pocket: a single center prospective study. Eur Rev Med Pharmacol Sci 24:991–999. https://doi.org/10.26355/eurrev_202002_20149
Kim Y-H, Yang Y-J, Lee D-W et al (2023) Prevention of postoperative complications by prepectoral versus subpectoral breast reconstruction: a systematic review and meta-analysis. Plast Reconstr Surg. https://doi.org/10.1097/prs.0000000000010493
Hassan AM, Asaad M, Morris N et al (2023) Subpectoral implant placement is not protective against postmastectomy radiotherapy-related complications compared to prepectoral placement. Plast Reconstr Surg. https://doi.org/10.1097/PRS.0000000000010489
Long C, Kraenzlin F, Aravind P et al (2022) Prepectoral breast reconstruction is safe in the setting of post-mastectomy radiation therapy. J Plast Reconstr Aesthet Surg 75:3041–3047. https://doi.org/10.1016/j.bjps.2022.04.030
Teotia SS, Amaya J, Haddock NT (2023) Impact of prepectoral versus subpectoral tissue expander placement on outcomes in delayed-immediate autologous patients who undergo postmastectomy radiation therapy. Plast Reconstr Surg 151:709e–718e. https://doi.org/10.1097/PRS.0000000000010068
Zheng C, Liu J, Wen Y et al (2022) A systematic review and meta-analysis of postmastectomy radiation therapy on prepectoral versus subpectoral breast reconstruction. Front Surg 9:1019950. https://doi.org/10.3389/fsurg.2022.1019950
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg 88:105906. https://doi.org/10.1016/j.ijsu.2021.105906
Wells G, Shea B, O’Connell D, et al (2020) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 30 Oct 2020
Patel AA, Arquette CP, Yesantharao PS et al (2021) Examining the effects of postmastectomy radiation therapy in prepectoral versus subpectoral autologous breast reconstruction. Ann Plast Surg 86:S390–S394. https://doi.org/10.1097/SAP.0000000000002762
Sinnott CJ, Persing SM, Pronovost M et al (2018) Impact of postmastectomy radiation therapy in prepectoral versus subpectoral implant-based breast reconstruction. Ann Surg Oncol 25:2899–2908. https://doi.org/10.1245/s10434-018-6602-7
Sbitany H, Piper M, Lentz R (2017) Prepectoral breast reconstruction: a safe alternative to submuscular prosthetic reconstruction following nipple-sparing mastectomy. Plast Reconstr Surg 140:432–443. https://doi.org/10.1097/PRS.0000000000003627
Sobti N, Weitzman RE, Nealon KP et al (2020) Evaluation of capsular contracture following immediate prepectoral versus subpectoral direct-to-implant breast reconstruction. Sci Rep 10:1137. https://doi.org/10.1038/s41598-020-58094-4
Thuman JM, Worbowtiz N, Jain A et al (2021) Impact of radiation on implant-based breast reconstruction in prepectoral versus submuscular planes. Ann Plast Surg 86:S560–S566. https://doi.org/10.1097/SAP.0000000000002882
Kraenzlin F, Darrach H, Khavanin N et al (2021) Tissue expander-based breast reconstruction in the prepectoral versus subpectoral plane: an analysis of short-term outcomes. Ann Plast Surg 86:19–23. https://doi.org/10.1097/SAP.0000000000002415
Schaeffer CV, Dassoulas KR, Thuman J, Campbell CA (2019) Early functional outcomes after prepectoral breast reconstruction: a case-matched cohort study. Ann Plast Surg 82:S399–S403. https://doi.org/10.1097/SAP.0000000000001669
Nigro LC, Blanchet NP (2017) Animation deformity in postmastectomy implant-based reconstruction. Plast Reconstr surgery Glob open 5:e1407. https://doi.org/10.1097/GOX.0000000000001407
Zhu L, Liu C (2023) Postoperative complications following prepectoral versus partial subpectoral implant-based breast reconstruction using adm: a systematic review and meta-analysis. Aesthetic Plast Surg 47:1260–1273. https://doi.org/10.1007/s00266-023-03296-0
Craig ES, Clemens MW, Koshy JC et al (2019) Outcomes of acellular dermal matrix for immediate tissue expander reconstruction with radiotherapy: a retrospective cohort study. Aesthetic Surg J 39:279–288. https://doi.org/10.1093/asj/sjy127
Komorowska-Timek E, Oberg KC, Timek TA et al (2009) The effect of AlloDerm envelopes on periprosthetic capsule formation with and without radiation. Plast Reconstr Surg 123:807–816. https://doi.org/10.1097/PRS.0b013e318199eef3
Frey JD, Salibian AA, Choi M, Karp NS (2017) Mastectomy flap thickness and complications in nipple-sparing mastectomy: objective evaluation using magnetic resonance imaging. Plast Reconstr surgery Glob open 5:e1439. https://doi.org/10.1097/GOX.0000000000001439
Sbitany H (2017) Important considerations for performing prepectoral breast reconstruction. Plast Reconstr Surg 140:7S-13S. https://doi.org/10.1097/PRS.0000000000004045
Salibian AA, Frey JD, Karp NS (2019) Strategies and considerations in selecting between subpectoral and prepectoral breast reconstruction. Gland Surg 8:11–18. https://doi.org/10.21037/gs.2018.08.01
Funding
None
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
None
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, X., Ning, S. & Zhang, Y. Complications After Prepectoral Versus Subpectoral Breast Reconstruction in Patients Receiving Postmastectomy Radiation Therapy: A Systematic Review and Meta-Analysis. Aesth Plast Surg (2024). https://doi.org/10.1007/s00266-024-04096-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00266-024-04096-w