Abstract
Background
Hyperpigmented scars, particularly in exposed body areas, can be difficult to conceal and may evoke psychological distress. While the precise causes of scar dyschromia are not fully understood, alterations in melanogenic activity appear to hold more significance than changes in melanocyte quantity. Current treatments encompass laser interventions. However, it is essential to consider their costs and potential complications in relation to their limited proven effectiveness. Fat grafting has gained interest as a scar modulation technique due to its regenerative properties, and its efficacy in reducing scar hyperpigmentation is currently under investigation.
Methods
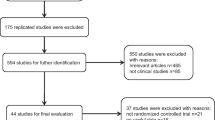
A systematic review and meta-analysis was reported according to PRISMA guidelines. PubMed, Embase, and Cochrane Library databases were accessed. PROSPERO registration number is CRD42023457778. The primary outcome was a change in scar pigmentation after fat grafting. Pigmentation changes after fat grafting were calculated using the standardized mean difference (SMD) between baseline and postoperative scores according to POSAS and VSS scales. Bias assessment was conducted according to the National Institute for Health and Clinical Excellence quality assessment tool.
Results
A total of 8 articles meeting inclusion and exclusion criteria were identified, involving 323 patients with hyperpigmented scars treated with fat grafting. A significant difference in scar pigmentation was noted after treatment with fat grafting according to observers’ ratings, with a SMD of − 1.09 [95% CI: − 1.32; − 0.85], p<0.01. The SMD for patient-reported scar pigmentation after treatment with fat grafting was − 0.99 [96% CI: − 1.31; − 0.66], p<0.01. Four studies provided objective measurements of melanin changes after fat grafting and revealed inconsistent findings compared to subjective observations.
Conclusions
Fat grafting shows promise in ameliorating hyperpigmented scars based on subjective assessments, but further corroborating evidence from objective measures is required.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.





Similar content being viewed by others
Change history
26 February 2024
A Correction to this paper has been published: https://doi.org/10.1007/s00266-024-03916-3
References
Travis TE, Ghassemi P, Ramella-Roman JC et al (2015) A multimodal assessment of melanin and melanocyte activity in abnormally pigmented hypertrophic scar. J Burn Care Res 36(1):77–86. https://doi.org/10.1097/BCR.0000000000000154
Velangi SS, Rees JL (2001) Why are scars pale? An immunohistochemical study indicating preservation of melanocyte number and function in surgical scars. Acta Derm Venereol 81(5):326–328. https://doi.org/10.1080/000155501317140016
Kurup S, Travis TE, Shafy RAE, Shupp JW, Carney BC (2023) Treatment of burn hypertrophic scar with fractional ablative laser-assisted drug delivery can decrease levels of hyperpigmentation. Lasers Surg Med 55(5):471–479. https://doi.org/10.1002/lsm.23662
Carney BC, Travis TE, Moffatt LT et al (2021) Hypopigmented burn hypertrophic scar contains melanocytes that can be signaled to re-pigment by synthetic alpha-melanocyte stimulating hormone in vitro. PLoS ONE 16(3):e0248985. https://doi.org/10.1371/journal.pone.0248985
Gao FL, Jin R, Zhang L, Zhang YG (2013) The contribution of melanocytes to pathological scar formation during wound healing. Int J Clin Exp Med 6(7):609–613
Amici JM, Cogrel O, Jourdan M et al (2023) Expert recommendations on supportive skin care for non-surgical and surgical procedures. J Eur Acad Dermatol Venereol 37(Suppl 3):16–33. https://doi.org/10.1111/jdv.18855
Leszczynski R, da Silva CA, Pinto ACPN, Kuczynski U, da Silva EM (2022) Laser therapy for treating hypertrophic and keloid scars. Cochrane Database Syst Rev 9(9):CD011642. https://doi.org/10.1002/14651858.CD011642.pub2
Al-Niaimi F (2016) Laser and energy-based devices’ complications in dermatology. J Cosmet Laser Ther 18(1):25–30. https://doi.org/10.3109/14764172.2015.1052511
Peng W, Zhang X, Kong X, Shi K (2021) The efficacy and safety of fractional CO2 laser therapy in the treatment of burn scars: a meta-analysis. Burns 47(7):1469–1477. https://doi.org/10.1016/j.burns.2021.08.010
Firriolo JM, Condé-Green A, Pu LLQ (2022) Fat grafting as regenerative surgery: a current review. Plast Reconstr Surg 150(6):1340e–1347e. https://doi.org/10.1097/PRS.0000000000009710
Han Y, Li X, Zhang Y, Han Y, Chang F, Ding J (2019) Mesenchymal stem cells for regenerative medicine. Cells 8(8):886. https://doi.org/10.3390/cells8080886
Egro FM, Roy E, Rubin JP, Coleman SR (2022) Evolution of the coleman technique. Plast Reconstr Surg 150(2):329e–336e. https://doi.org/10.1097/PRS.0000000000009355
Khouri RK, Khouri RK (2017) Current clinical applications of fat grafting. Plast Reconstr Surg 140(3):466e–486e. https://doi.org/10.1097/PRS.0000000000003648
Alessandri-Bonetti M, Egro FM, Persichetti P, Coleman SR, Peter RJ (2019) The role of fat grafting in alleviating neuropathic pain: a critical review of the literature. Plast Reconstr Surg Glob Open 7(5):e2216. https://doi.org/10.1097/GOX.0000000000002216
Tran VVT, Jin X, Hong KY, Chang H (2023) Effects of nanofat in plastic and reconstructive surgery: a systematic review. Plast Reconstr Surg. https://doi.org/10.1097/PRS.0000000000010905
Negenborn VL, Groen JW, Smit JM, Niessen FB, Mullender MG (2016) The use of autologous fat grafting for treatment of scar tissue and scar-related conditions: a systematic review. Plast Reconstr Surg 137(1):31e–43e. https://doi.org/10.1097/PRS.0000000000001850
Alessandri-Bonetti M, Coscarella G, Amendola F et al (2023) The use of adipose tissue-based therapies on facial atrophic postacne vulgaris scars. Facial Plast Surg Aesthet Med. https://doi.org/10.1089/fpsam.2023.0103
Gentile P, Scioli MG, Bielli A, Orlandi A, Cervelli V (2017) Concise review: the use of adipose-derived stromal vascular fraction cells and platelet rich plasma in regenerative plastic surgery. Stem Cells 35(1):117–134. https://doi.org/10.1002/stem.2498
Bora P, Majumdar AS (2017) Adipose tissue-derived stromal vascular fraction in regenerative medicine: a brief review on biology and translation. Stem Cell Res Ther 8(1):145. https://doi.org/10.1186/s13287-017-0598-y
Zuk PA, Zhu M, Ashjian P et al (2002) Human adipose tissue is a source of multipotent stem cells. Mol Biol Cell 13(12):4279–4295. https://doi.org/10.1091/mbc.e02-02-0105
Zuk PA, Zhu M, Mizuno H et al (2001) Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng 7(2):211–228. https://doi.org/10.1089/107632701300062859
Tonnard P, Verpaele A, Carvas M (2020) Fat grafting for facial rejuvenation with nanofat grafts. Clin Plast Surg 47(1):53–62. https://doi.org/10.1016/j.cps.2019.08.006
van Dongen JA, Langeveld M, van de Lande LS, Harmsen MC, Stevens HP, van der Lei B (2019) The effects of facial lipografting on skin quality: a systematic review. Plast Reconstr Surg 144(5):784e–797e. https://doi.org/10.1097/PRS.0000000000006147
Tonnard P, Verpaele A, Carvas M (2020) Fat grafting for facial rejuvenation with nanofat grafts. Clin Plast Surg 47(1):53–62. https://doi.org/10.1016/j.cps.2019.08.006
Bashir A, Bashir MM, Sohail M, Choudhery MS (2020) Adipose tissue grafting improves contour deformities related hyperpigmentation of face. J Craniofac Surg 31(5):1228–1231. https://doi.org/10.1097/SCS.0000000000006377
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Amir-Behghadami M, Janati A (2020) Population, intervention, comparison, outcomes and study (PICOS) design as a framework to formulate eligibility criteria in systematic reviews. Emerg Med J 37(6):387. https://doi.org/10.1136/emermed-2020-209567
van de Kar AL, Corion LUM, Smeulders MJC, Draaijers LJ, van der Horst CMAM, van Zuijlen PPM (2005) Reliable and feasible evaluation of linear scars by the patient and observer scar assessment scale. Plast Reconstr Surg 116(2):514–522. https://doi.org/10.1097/01.prs.0000172982.43599.d6
Baryza MJ, Baryza GA (1995) The Vancouver scar scale: an administration tool and its interrater reliability. J Burn Care Rehabil 16(5):535–538. https://doi.org/10.1097/00004630-199509000-00013
National Heart, Lung, and Blood Institute (2021) Study quality assessment tools. National Institutes of Health. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed August 16, 2023
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds) (2023) Cochrane handbook for systematic reviews of interventions. https://training.cochrane.org/handbook. Accessed August 16, 2023
Alessandri-Bonetti M, Costantino A, Gallo Afflitto G et al (2022) Anxiety and depression mood disorder in patients with nasal septal deviation: a systematic review and meta-analysis. Am J Otolaryngol 43(5):103517. https://doi.org/10.1016/j.amjoto.2022.103517
Gallo Afflitto G, Chou TH, Swaminathan SS et al (2023) Pattern electroretinogram in ocular hypertension, glaucoma suspect and early manifest glaucoma eyes: a systematic review and meta-analysis. Ophthalmol Sci. 3(4):100322. https://doi.org/10.1016/j.xops.2023.100322
Hedges LV (1981) Distribution theory for glass’s estimator of effect size and related estimators. J Educ Stat 6(2):107–128. https://doi.org/10.3102/10769986006002107
Cochran WG (1954) The combination of estimates from different experiments. Biometrics 10(1):101–129. https://doi.org/10.2307/3001666
Jackson D, White IR, Riley RD (2012) Quantifying the impact of between-study heterogeneity in multivariate meta-analyses. Stat Med 31(29):3805–3820. https://doi.org/10.1002/sim.5453
Brown JC, Shang H, Yang N et al (2020) Autologous fat transfer for scar prevention and remodeling: a randomized, blinded, placebo-controlled trial. Plast Reconstr Surg Glob Open 8(5):e2830. https://doi.org/10.1097/GOX.0000000000002830
Ghareeb F et al (2017) Improving esthetic outcome of facial scars by fat grafting. Menoufia Med J 30(2):412–419. https://www.mmj.eg.net/article.asp?issn=1110-2098;year=2017;volume=30;issue=2;spage=412;epage=419;aulast=Ghareeb. Accessed August 18, 2023
Jan SN, Bashir MM, Khan FA et al (2019) Unfiltered nanofat injections rejuvenate postburn scars of face. Ann Plast Surg 82(1):28–33. https://doi.org/10.1097/SAP.0000000000001631
Jaspers MEH, Brouwer KM, van Trier AJM, Middelkoop E, van Zuijlen PPM (2017) Sustainable effectiveness of single-treatment autologous fat grafting in adherent scars. Wound Repair Regen 25(2):316–319. https://doi.org/10.1111/wrr.12521
Juhl AA, Karlsson P, Damsgaard TE (2016) Fat grafting for alleviating persistent pain after breast cancer treatment: a randomized controlled trial. J Plast Reconstr Aesthet Surg 69(9):1192–1202. https://doi.org/10.1016/j.bjps.2016.07.003
Sardesai MG, Moore CC (2007) Quantitative and qualitative dermal change with microfat grafting of facial scars. Otolaryngol Head Neck Surg 137(6):868–872. https://doi.org/10.1016/j.otohns.2007.08.008
Bruno A, Delli Santi G, Fasciani L, Cempanari M, Palombo M, Palombo P (2013) Burn scar lipofilling: immunohistochemical and clinical outcomes. J Craniofac Surg 24(5):1806–1814. https://doi.org/10.1097/SCS.0b013e3182a148b9
Dai Q, Yu Q, Xiao R, Cai L (2021) Early intervention with autologous fat grafting to reduce hypertrophic scar formation: a prelimilary study. Aesthetic Plast Surg 45(5):2409–2416. https://doi.org/10.1007/s00266-021-02277-5
Muffley LA, Zhu KQ, Engrav LH, Gibran NS, Hocking AM (2011) Spatial and temporal localization of the melanocortin 1 receptor and its ligand α-melanocyte-stimulating hormone during cutaneous wound repair. J Histochem Cytochem 59(3):278–288. https://doi.org/10.1369/0022155410397999
Seo SR, Kang NO, Yoon MS, Lee HJ, Kim DH (2017) Measurements of scar properties by SkinFibroMeter®, SkinGlossMeter®, and Mexameter® and comparison with Vancouver scar scale. Skin Res Technol 23(3):295–302. https://doi.org/10.1111/srt.12334
Jatin B, Karki D, Ahluwalia C, Muthukumar V, Karki D (2023) Lipofilling-a regenerative alternate for remodeling burn scars: a clinico-immunohistopathological study. Indian J Plast Surg 56(4):357–366. https://doi.org/10.1055/s-0043-1771515
Klar AS, Biedermann T, Michalak K et al (2017) Human adipose mesenchymal cells inhibit melanocyte differentiation and the pigmentation of human skin via increased expression of TGF-β1. J Invest Dermatol 137(12):2560–2569. https://doi.org/10.1016/j.jid.2017.06.027
Shen JP, Wu YX, Tang SJ, Peng LH (2022) Experimental study on stromal vascular fraction mediated inhibition of skin pigmentation in guinea pigs. Ann Transl Med 10(23):1268. https://doi.org/10.21037/atm-22-5433
Kim KH, Lee S, Bae S (2023) Whitening and moisturizing enhancing effects of three-dimensional human adipose-derived mesenchymal stem cell-conditioned medium-containing cream. J Cosmet Dermatol. https://doi.org/10.1111/jocd.15879
Raktoe R, Kwee AKAL, Rietveld M et al (2023) Mimicking fat grafting of fibrotic scars using 3D-organotypic skin cultures. Exp Dermatol 32(10):1752–1762. https://doi.org/10.1111/exd.14893
Nilforoushzadeh MA, Heidari-Kharaji M, Alavi S et al (2022) Transplantation of autologous fat, stromal vascular fraction (SVF) cell, and platelet-rich plasma (PRP) for cell therapy of atrophic acne scars: clinical evaluation and biometric assessment. J Cosmet Dermatol 21(5):2089–2098. https://doi.org/10.1111/jocd.14333
Gentile P (2023) Lipofilling enriched with adipose-derived mesenchymal stem cells improves soft tissue deformities and reduces scar pigmentation: clinical and instrumental evaluation in plastic surgery. Aesthetic Plast Surg. https://doi.org/10.1007/s00266-023-03325-y
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest to disclose.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors
Informed Consent
For this type of study, informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alessandri Bonetti, M., Arellano, J.A., Scarabosio, A. et al. The Effect of Fat Grafting on Scars Hyperpigmentation: A Systematic Review and Meta-Analysis. Aesth Plast Surg 48, 989–998 (2024). https://doi.org/10.1007/s00266-023-03828-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-023-03828-8