Abstract
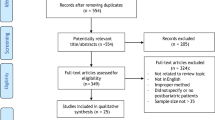
With the increase in obesity prevalence, a noticeable increase in bariatric surgeries has been reported in national and international statistics. Therefore, body contouring surgeries have increased to help individuals achieve their desired body shape. Plastic surgeons need to consider potential hematologic complications that may occur in this specific group of patients before performing body contouring surgery. This review illustrates the perioperative medical, laboratory, and management strategies needed to minimize blood loss and blood transfusion requirements during body contouring. Using Google Scholar and PubMed, a comprehensive literature review was conducted to identify articles discussing post-bariatric body contouring perioperative blood management strategies, including the effects of bariatric surgery on hemostasis as well as basic hematology and coagulation. In preoperative blood management, blood investigations aid in the early detection of electrolytes, protein, and vitamin deficiencies and anemia, resulting in the early correction of nutritional deficiencies. In order to reduce postoperative complications, surgical and anesthesia techniques, as well as intraoperative pharmacological therapy, play an essential role. Postoperative blood transfusion and restrictive transfusion thresholds are tailored to the patient's needs and depend on various physiological indicators, such as heart rate, blood pressure, urine output, and laboratory findings, such as acidosis and hematocrit level. Generally, post-bariatric body contouring blood management measures are still lacking, and more research is required to develop standardized guidelines for optimizing patient safety and satisfaction.
Level of Evidence III This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.


Similar content being viewed by others
References
Clinical Guidelines on the Identification (1998) Evaluation, and treatment of overweight and obesity in adults-the evidence report. Natl Inst Health Obes Res 6(Suppl 2):51S-209S
Santry HP, Gillen DL, Lauderdale DS (2005) Trends in bariatric surgical procedures. JAMA 294(15):1909–1917
Vuong L et al (2022) National trends and outcomes in adolescents undergoing bariatric surgery. J Am Coll Surg 235(2):186–194
Khorgami Z et al (2019) Outcomes of bariatric surgery versus medical management for type 2 diabetes mellitus: a meta-analysis of randomized controlled trials. Obes Surg 29(3):964–974
Hall JC et al (1990) Gastric surgery for morbid obesity. The adelaide study. Ann Surg 211(4):419–427
Nguyen NT et al (2001) Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg 234(3):279–389
Pories WJ et al (1995) Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg 222(3):339–350
Sugerman HJ et al (2003) Diabetes and hypertension in severe obesity and effects of gastric bypass-induced weight loss. Ann Surg 237(6):751–756
Buchwald H et al (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292(14):1724–1737
Christou NV et al (2004) Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg 240(3):416–23
Welbourn R et al (2019) Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the fourth ifso global registry report 2018. Obes Surg 29(3):782–795
Ellison JM, Steffen KJ, Sarwer DB (2015) Body contouring after bariatric surgery. Eur Eat Disord Rev 23(6):479–487
Shermak MA et al (2006) An outcomes analysis of patients undergoing body contouring surgery after massive weight loss. Plast Reconstr Surg 118(4):1026–1031
Clements RH et al (2006) Incidence of vitamin deficiency after laparoscopic roux-en-Y gastric bypass in a university hospital setting. Am Surg 72(12):1196–202
O’Kane M (2021) Nutritional consequences of bariatric surgery–prevention, detection and management. Curr Opin Gastroenterol 37(2):135–144
Matarasso A et al (2007) Bariatric surgery: an overview of obesity surgery. Plast Reconstr Surg 119(4):1357–1362
Love AL, Billett HH (2008) Obesity, bariatric surgery, and iron deficiency: true, true, true and related. Am J Hematol 83(5):403–409
Stassen JM, Arnout J, Deckmyn H (2004) The hemostatic system. Curr Med Chem 11(17):2245–2260
Mackman N, Tilley RE, Key NS (2007) Role of the extrinsic pathway of blood coagulation in hemostasis and thrombosis. Arterioscler Thromb Vasc Biol 27(8):1687–1693
Bladbjerg EM, Stolberg CR, Juhl CB (2020) Effects of obesity surgery on blood coagulation and fibrinolysis: a literature review. Thromb Haemost 120(4):579–591
Chapin JC, Hajjar KA (2015) Fibrinolysis and the control of blood coagulation. Blood Rev 29(1):17–24
Chen M et al (2013) Hematological disorders following gastric bypass surgery: emerging concepts of the interplay between nutritional deficiency and inflammation. Biomed Res Int 2013:205467
Ay L et al (2016) Decrease in microvesicle-associated tissue factor activity in morbidly obese patients after bariatric surgery. Int J Obes 40(5):768–772
Primrose JN et al (1992) Reduction in factor VII, fibrinogen and plasminogen activator inhibitor-1 activity after surgical treatment of morbid obesity. Thromb Haemost 68(4):396–399
Lupoli R et al (2015) Haemostatic and fibrinolytic changes in obese subjects undergoing bariatric surgery: the effect of different surgical procedures. Blood Transfus 13(3):442–447
Stolberg CR et al (2018) Effects of gastric bypass surgery followed by supervised physical training on inflammation and endothelial function: a randomized controlled trial. Atherosclerosis 273:37–44
American Society of Anesthesiologists Task Force on Perioperative Blood (2015) Practice guidelines for perioperative blood management: an updated report by the american society of anesthesiologists task force on perioperative blood management*. Anesthesiology 122(2): 241–75
Alwasaidi TA et al (2020) Determining the prevalence and causes of anaemia in patients after bariatric surgery in a Saudi hospital. J Taibah Univ Med Sci 15(2):129–135
Richards T et al (2020) Preoperative intravenous iron to treat anaemia before major abdominal surgery (PREVENTT): a randomised, double-blind, controlled trial. Lancet 396(10259):1353–1361
Fowler AJ et al (2015) Meta-analysis of the association between preoperative anaemia and mortality after surgery. Br J Surg 102(11):1314–1324
Enrique Bayter-Marin J et al (2021) Patient blood management strategies to avoid transfusions in body contouring operations: controlled clinical trial. Plast Reconstr Surg 147(2):355–363
von Drygalski A et al (2011) Anemia after bariatric surgery cannot be explained by iron deficiency alone: results of a large cohort study. Surg Obes Relat Dis 7(2):151–156
Majumder S et al (2013) Vitamin B12 deficiency in patients undergoing bariatric surgery: preventive strategies and key recommendations. Surg Obes Relat Dis 9(6):1013–1019
Goodnough LT et al (2011) Detection, evaluation, and management of preoperative anaemia in the elective orthopaedic surgical patient: NATA guidelines. Br J Anaesth 106(1):13–22
Munoz M et al (2017) International consensus statement on the peri-operative management of anaemia and iron deficiency. Anaesthesia 72(2):233–247
Meybohm P et al (2017) “Simplified international recommendations for the implementation of patient blood management” (SIR4PBM). Perioper Med 6:5
Khalafallah AA et al (2016) Intravenous ferric carboxymaltose versus standard care in the management of postoperative anaemia: a prospective, open-label, randomised controlled trial. Lancet Haematol 3(9):e415–e425
Unger EF et al (2010) Erythropoiesis-stimulating agents–time for a reevaluation. N Engl J Med 362(3):189–192
Naghshineh N et al (2010) Nutritional assessment of bariatric surgery patients presenting for plastic surgery: a prospective analysis. Plast Reconstr Surg 126(2):602–610
Rubin JP, Nguyen V, Schwentker A (2004) Perioperative management of the post-gastric-bypass patient presenting for body contour surgery. Clin Plast Surg 31(4):601–610
Aarts EO et al (2012) Prevalence of anemia and related deficiencies in the first year following laparoscopic gastric bypass for morbid obesity. J Obes 2012:193705
Lespessailles E, Toumi H (2017) Vitamin D alteration associated with obesity and bariatric surgery. Exp Biol Med 242(10):1086–1094
Kuin C et al (2019) Treatment of severe protein malnutrition after bariatric surgery. Obes Surg 29(10):3095–3102
Colwell AS, Borud LJ (2008) Optimization of patient safety in postbariatric body contouring: a current review. Aesthet Surg J 28(4):437–442
van der Beek ES, van der Molen AM, van Ramshorst B (2011) Complications after body contouring surgery in post-bariatric patients: the importance of a stable weight close to normal. Obes Facts 4(1):61–66
Colwell AS (2010) Current concepts in post-bariatric body contouring. Obes Surg 20(8):1178–1182
Arthurs ZM et al (2007) Post-bariatric panniculectomy: pre-panniculectomy body mass index impacts the complication profile. Am J Surg 193(5):567–570
Au K et al (2008) Correlation of complications of body contouring surgery with increasing body mass index. Aesthet Surg J 28(4):425–429
Coon D et al (2012) Hypothermia and complications in postbariatric body contouring. Plast Reconstr Surg 130(2):443–448
Shermak MA (2012) Pearls and perils of caring for the postbariatric body contouring patient. Plast Reconstr Surg 130(4):585e–596e
Klein JA (1990) Tumescent technique for regional anesthesia permits lidocaine doses of 35 mg/kg for liposuction. J Dermatol Surg Oncol 16(3):248–263
Soueid A, Nawinne M, Khan H (2008) Randomized clinical trial on the effects of the use of diluted adrenaline solution in reduction mammaplasty: same patient, same technique, same surgeon. Plast Reconstr Surg 121(3):30e–33e
Holzman NL, et al., (2015) Use of tumescence for outpatient abdominoplasty and other concurrent body contouring procedures: a review of 65 consecutive patients. Eplasty 15
Kim H et al (2020) Usage of epinephrine mixed with lidocaine in plastic surgery. J Craniofac Surg 31(3):791–793
Serrano Reyes HM et al (2021) Tranexamic acid: a simple way to reduce drainage and bleeding in rhytidoplasty. Eur J Plast Surg 44(2):189–196
McCormack PL (2012) Tranexamic acid: a review of its use in the treatment of hyperfibrinolysis. Drugs 72(5):585–617
Verstraete M (1985) Clinical application of inhibitors of fibrinolysis. Drugs 29(3):236–261
Ng W, Jerath A, Wąsowicz M (2015) Tranexamic acid: a clinical review. Anaesthesiol Intensive Ther 47(4):339–350
Soslau G, Horrow J, Brodsky I (1991) Effect of tranexamic acid on platelet ADP during extracorporeal circulation. Am J Hematol 38(2):113–119
Wong D, Lam TK (2022) The role of tranexamic acid in breast and body contouring surgery: a review of the literature. Australas J Plast Surg 5(1):24–31
Ausen K et al (2019) Serum concentrations and pharmacokinetics of tranexamic acid after two means of topical administration in massive weight loss skin-reducing surgery. Plast Reconstr Surg 143(6):1169e–1178e
Laikhter E et al (2022) A systematic review and meta-analysis evaluating the impact of tranexamic acid administration in aesthetic plastic surgery. Aesthet Surg J 42(5):548–558
Yin C et al (2021) Body contouring in massive weight loss patients receiving venous thromboembolism chemoprophylaxis: a systematic review. Plast Reconstr Surg Glob Open 9(8):e3746
Devereaux PJ et al (2022) Tranexamic acid in patients undergoing noncardiac surgery. N Engl J Med 386(21):1986–1997
Schulte J et al (2005) Developmental outcome of the use of etamsylate for prevention of periventricular haemorrhage in a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed 90(1):F31–F35
Elbourne D et al (2001) Randomised controlled trial of prophylactic etamsylate: follow up at 2 years of age. Arch Dis Child Fetal Neonatal Ed 84(3):F183–F187
Kovács L, Falkay G (1981) Etamsylate as inhibitor of prostaglandin biosynthesis in pregnant human myometrium in vitro. Experientia 37(11):1182–1183
Harrison RF, Cambell S (1976) A double-blind trial of ethamsylate in the treatment of primary and intrauterine-device menorrhagia. Lancet 2(7980):283–285
Torky H et al (2021) Pre-operative tranexemic acid versus etamsylate in reducing blood loss during elective cesarean section: randomized controlled trial. J Perinat Med 49(3):353–356
Fakih-Gomez N et al (2021) Postoperative ecchymosis in upper blepharoplasty: a split face study of tranexamic acid versus etamsylate. Am J Cosmet Surg. https://doi.org/10.1177/07488068211059009
Bloom JA et al (2021) The use of hemostatic agents to decrease bleeding complications in general plastic surgery procedures. Plast Reconstr Surg Glob Open 9(8):e3744
Rudolph M et al (2019) Lymphostasis and hemostasis in body-contouring surgery using a polysaccharide based hemostat (4DryField PH). Plast Reconstr Surg Glob Open 7(3):e2128
McGohan LD (2007) Body contouring following major weight loss. J Contin Educ Nurs 38(3):103–104
Wolf AM, Kuhlmann HW (2007) Reconstructive procedures after massive weight loss. Obes Surg 17(3):355–360
Espinosa-de-los-Monteros A et al (2006) Abdominoplasty with total abdominal liposuction for patients with massive weight loss. Aesthetic Plast Surg 30(1):42–46
Marouf A, Mortada H (2021) Complications of body contouring surgery in postbariatric patients: a systematic review and meta-analysis. Aesthetic Plast Surg 45(6):2810–2820
Souto LR et al (2012) Increased intraoperative bleeding in patients undergoing abdominoplasty after gastroplasty is not due to coagulopathy. Aesthetic Plast Surg 36(6):1283–1291
Gando S, Tedo I, Kubota M (1992) Posttrauma coagulation and fibrinolysis. Crit Care Med 20(5):594–600
Cosgriff N et al (1997) Predicting life-threatening coagulopathy in the massively transfused trauma patient: hypothermia and acidoses revisited. J Trauma 42(5):857–861
Shander A et al (2011) What is really dangerous: anaemia or transfusion? Br J Anaesth 107(Suppl 1):i41-59
Bernard AC et al (2009) Intraoperative transfusion of 1 U to 2 U packed red blood cells is associated with increased 30-day mortality, surgical-site infection, pneumonia, and sepsis in general surgery patients. J Am Coll Surg 208(5):931–937
Oliver E et al (2009) Relationships among haemoglobin level, packed red cell transfusion and clinical outcomes in patients after cardiac surgery. Intensive Care Med 35(9):1548–1555
Beattie WS et al (2009) Risk associated with preoperative anemia in noncardiac surgery: a single-center cohort study. J Am Soc Anesthesiol 110(3):574–581
Masoomi H et al (2014) Frequency and risk factors of blood transfusion in abdominoplasty in post-bariatric surgery patients. Plast Reconstr Surg 134(4S–1):105–106
Van Walraven C, Dhalla IA, Bell C, Etchells E, Stiell IG, Zarnke K et al (2010) Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. C Can Med Assoc J 182:551. https://doi.org/10.1503/CMAJ.091117
Winter E, Glauser G, Caplan IF, Goodrich S, McClintock SD, Kovach SJ et al (2020) The LACE+ index as a predictor of 30-day patient outcomes in a plastic surgery population: a coarsened exact match study. Plast Reconstr Surg. https://doi.org/10.1097/PRS.0000000000007064
Guarro G, Cozzani F, Rossini M, Bonati E, Del Rio P (2021) The modified time-h scoring system, a versatile tool in wound management practice: a preliminary report. Acta Biomed. https://doi.org/10.23750/abm.v92i4.10666
Lim K, Free B, Sinha S (2015) Modified TIME-H: a simplified scoring system for chronic wound management. J Wound Care 24:415–419. https://doi.org/10.12968/JOWC.2015.24.9.415
Boissiere F, Gandolfi S, Riot S, Kerfant N, Jenzeri A, Hendriks S et al (2021) Flap venous congestion and salvage techniques: a systematic literature review. Plast Reconstr Surg Glob Open 9:e3327. https://doi.org/10.1097/GOX.0000
Acknowledgment
This work was supported by the College of Medicine Research Center, Deanship of Scientific Research, King Saud University Medical City, King Saud University, Riyadh, Saudi Arabia.
Funding
The authors do not have any conflict of funding to declare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors do not have any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Neel, O.F., Mortada, H., Qasim, S.S. et al. Current Practices and Guidelines for Perioperative Blood Management in Post-Bariatric Body Contouring Surgery: A Comprehensive Review of Literature. Aesth Plast Surg 47, 1462–1471 (2023). https://doi.org/10.1007/s00266-022-03192-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-022-03192-z