Abstract
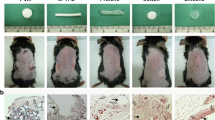
Polymethylmethacrylate (PMMA) is a filler used for aesthetic and/or repair purposes. The response to the implantation of biomaterials varies according to factors related to the patient, the professional responsible for the application and the material used. In vitro and in vivo experimental models have been used to study aspects such as the organism/biomaterial interface and the role of macrophages, dendritic cells and neutrophils. This study aimed to characterize the inflammatory reactions related to polymer concentration, implantation depth and exposure time. Different concentrations of PMMA were implanted in different anatomical planes in mice. The consequences of contact with PMMA, from structural changes to the inflammatory characteristic of tissue damage, were histologically evaluated. The implantation interfered in the morphological structure of the region where it was implanted, expanding it and due to the inflammatory reaction generated, by the presence of the vehicle in the initial phase and by the collagen produced in the chronic phase. The 30% concentration of PMMA induced a greater presence of foreign body giant cells both subcutaneously, at 7, 30 and 90 days after implantation (DAI), and intramuscular at 30DAI. Tissue remodeling was more expressive in the subcutaneous region with significant density of the extracellular matrix at 90DAI. In conclusion, the foreign body reaction resulting from the implantation process acquires different characteristics depending on the anatomical plane and the concentration of implanted product, where the more superficial the implantation plane, the greater the inflammatory reaction. Moreover, PMMA concentration and the depth of implantation did not influence the collagen production.
No Level Assigned This journal requires that authors assign a level of evidence to each submission to which Evidence-Based Medicine rankings are applicable. This excludes Review Articles, Book Reviews, and manuscripts that concern Basic Science, Animal Studies, Cadaver Studies, and Experimental Studies. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors https://www.springer.com/00266





Similar content being viewed by others
References
Ali U, Karim KJBA, Buang NA (2015) A review of the properties and applications of poly (Methylmethacrylate) (PMMA). Polym Rev 55:678–705
Abdo Filho RCC, Oliveira TM, Lourenço Neto N et al (2011) Reconstruction of bony facial contour deficiencies with polymethylmethacrylate implants: case report. J Appl Oral Sci 19:426–430
Kwarcinski J, Boughton P, Ruys A et al (2017) Cranioplasty and craniofacial reconstruction: a review of implant material, manufacturing method and infection risk. Appl Sci 7:276
Milhomem AC, de Jorge IMS, da Costa EL et al (2020) Polymethylmethacrylate (PMMA) in the treatment of a case of hemifacial microsomia. Aesthetic Surg J Open Forum 2:1–5
Jones D (2005) HIV facial lipoatrophy: causes and treatment options. Dermatol Surg 31:1519–1529
Sun HL, Li CD, Yang ZC et al (2016) Polymethylmethacrylate augmentation of bone cement-injectable cannulated pedicle screws for the treatment of degenerative lumbar diseases with osteoporosis. Beijing Da Xue Xue Bao 48:1019–1025
Xu X, He L, Zhu B et al (2017) Advances in polymeric materials for dental applications. Polym Chem 8:807–823
Grzybowski A, Wasinska-Borowiec W, Alio JL et al (2017) Intraocular lenses in age-related macular degeneration. Graefe’s Arch Clin Exp Ophthalmol 255:1687–1696
Casavantes L, Lemperle G, Morales P (2016) Penile girth enhancement with Polymethylmethacrylate-based soft tissue fillers. J Sex Med 13:1414–1422
Romero-Otero J, Manfredi C, Ralph D et al (2021) Non-invasive and surgical penile enhancement interventions for aesthetic or therapeutic purposes: a systematic review. BJU Int 127:269–291
McCarthy CM, VanLaeken N, Lennox P et al (2010) The efficacy of Artecoll injections for the augmentation of nipple projection in breast reconstruction. Eplasty 10:e7
Lemperle G, Knapp TR, Sadick NS et al (2010) ArteFill® permanent injectable for soft tissue augmentation: I. Mechanism of action and injection techniques. Aesthetic Plast Surg 34:264–272
Lemperle G, Knapp TR, Sadick NS et al (2010) ArteFill® permanent injectable for soft tissue augmentation: II. Indications and applications. Aesthetic Plast Surg 34:273–286
Solomon P, Sklar M, Zener R (2012) Facial soft tissue augmentation with Artecoll®: a review of eight years of clinical experience in 153 patients. Can J Plast Surg 20:28–32
Li D, Luo S-K, Wang Y-C et al (2017) Facial volume restoration with permanent dermal filler (Artecoll-4) in Chinese women. Facial Plast Surg 33:537–544
Solomon P, Ng CL, Kerzner J et al (2021) Facial soft tissue augmentation with bellafill: a review of 4 years of clinical experience in 212 patients. Plast Surg (Oakv) 29:98–102
Klopfleisch R, Jung F (2017) The pathology of the foreign body reaction against biomaterials. J Biomed Mater Res Part A 105:927–940
Veiseh O, Vegas AJ (2019) Domesticating the foreign body response: recent advances and applications. Adv Drug Deliv Rev 144:148–161
Franz S, Rammelt S, Scharnweber D et al (2011) Immune responses to implants—a review of the implications for the design of immunomodulatory biomaterials. Biomaterials 32:6692–6709
De Boulle K, Heydenrych I (2015) Patient factors influencing dermal filler complications: prevention, assessment, and treatment. Clin Cosmet Investig Dermatol 8:205–214
Montealegre G, Uribe R, Martínez-Ceballos MA et al (2021) ASIA syndrome symptoms induced by gluteal biopolymer injections: case-series and narrative review. Toxicol Rep 8:303–314
Lemperle G (2018) Biocompatibility of injectable microspheres. Biomed J Sci Tech Res 2:2296–2306
Lemperle G, Gauthier-Hazan N, Wolters M et al (2009) Foreign body granulomas after all injectable dermal fillers: part 1. Possible causes. Plast Reconstr Surg 123:1842–1863
Carlos-Fabuel L, Marzal-Gamarra C, Martí-Álamo S et al (2012) Foreign body granulomatous reactions to cosmetic fillers. J Clin Exp Dent 4:e244
Paulucci BP (2020) PMMA safety for facial filling: review of rates of granuloma occurrence and treatment methods. Aesthetic Plast Surg 44:148–159
DeLorenzi C (2013) Complications of injectable fillers Part I. Aesthetic Surg J 33:561–575
Alijotas-Reig J, Fernández-Figueras MT, Puig L (2013) Late-onset inflammatory adverse reactions related to soft tissue filler injections. Clin Rev Allergy Immunol 45:97–108
Funt D, Pavicic T (2013) Dermal fillers in aesthetics: an overview of adverse events and treatment approaches. Clin Cosmet Investig Dermatol 6:295–316
Haneke E (2019) Adverse effects of fillers. Dermatol Ther 32:e12676
Costa EL, Milhomem AC, De Moura Filho RM et al (2016) Polymethyl methacrylate (Linnea Safe) causes local inflammatory response after intramuscular implant in BALB/c mice but it is not observed in distant organs. J Bras Patol e Med Lab 52:400–406
d’Eça NR, Herdt MA, Wohlgemuth FB et al (2012) Possible migration and histopathological analysis of injections of Polymethylmethacrylate in Wistar rats. ISRN Dermatol 2012:1–9
Lemperle G, Morhenn VB, Pestonjamasp V et al (2004) Migration studies and histology of injectable microspheres of different sizes in mice. Plast Reconstr Surg 113:1380–1390
Jhunjhunwala S, Aresta-DaSilva S, Tang K et al (2015) Neutrophil responses to sterile implant materials. PLoS ONE 10:e0137550
Jesus LH, Hildebrand LC, Martins MD et al (2015) Location of injected polymethylmethacrylate microspheres influences the onset of late adverse effects: an experimental and histopathologic study. Clin Cosmet Investig Dermatol 8:431–436
Moure SP, De Vargas KF, Borghetti RL et al (2012) Clinical and pathological characteristics of polymethylmethacrylate and hyaluronic acid in the rat tongue. Int J Oral Maxillofac Surg 41:1296–1303
Hubrecht RC, Carter E (2019) The 3Rs and humane experimental technique: implementing change. Animals (Basel) 9(10):754. https://doi.org/10.3390/ani9100754
Christo SN, Diener KR, Bachhuka A et al (2015) Innate immunity and biomaterials at the nexus: friends or foes. Biomed Res Int 2015:342604
Brooks PJ, Glogauer M, McCulloch CA (2019) An overview of the derivation and function of multinucleated giant cells and their role in pathologic processes. Am J Pathol 189:1145–1158
Miron RJ, Bosshardt DD (2018) Multinucleated giant cells: good guys or bad guys? Tissue Eng Part B Rev 24:53–65
Dondossola E, Holzapfel BM, Alexander S et al (2016) Examination of the foreign body response to biomaterials by nonlinear intravital microscopy. Nat Biomed Eng 1:0007
Funding
This study was funded by Company Bioplasty Brasil—Protocol No. 01/2017; Coordination for the Improvement of Higher Education Personnel—Brazil (CAPES)—Protocol Number: 88882.461654/2019-01.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest to disclose.
Human and animal rights
Animal rights were completely respected and this study followed the regulations of the ethical committee in animal use, approval protocol number 027/2017 (CEUA/UFG).
Informed consent
For this type of study, informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Milhomem, A.C., de Souza Jorge, I.M., dos Santos Arruda, F. et al. Tissue Remodeling After Implantation with Polymethylmethacrylate: An Experimental Study in Mice. Aesth Plast Surg 47, 1205–1216 (2023). https://doi.org/10.1007/s00266-022-03179-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-022-03179-w