Abstract
Background
Body contouring procedures provide patients with a meaningful improvement in health-related quality of life (QoL). We aim to compare the difference between the QoL in patients undergoing a single post-bariatric abdominal body contouring procedure (BCP) and those undergoing two or more concurrent procedures.
Methods and Materials
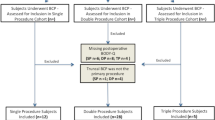
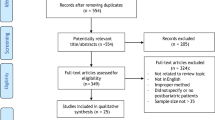
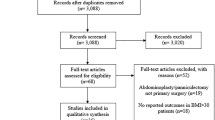
Patients evaluated for post-bariatric BCP were identified and administered the BODY-Q©. Patient demographics, clinical and operative characteristics, surgical outcomes, cost data, and absolute change in QoL scores were analyzed using descriptive statistics, chi-square, and Mann–Whitney U-test, between patients who underwent single (SP), double (DP), or triple (TP) concurrent procedures.
Results
A total of 45 patients were included. The median age was 52 years old ([IQR] ± 13). The majority were female (71.1%) and African-American (55.5%). The most common single procedure was panniculectomy (75%). Surgical site occurrences, readmissions, and the complication composite outcome did not differ between groups (p>0.05). No difference was seen between SP and DP QoL score (p>0.05). The DP had a statistically lower net QoL score compared with TP cohort in four domains. The SP had a statistically lower net QoL score compared with the TP in three domains. Average total cost for patients receiving an SP was $8,048.44, compared with $19,063.94 for DP (p<0.01), and $19,765.02 for TP (p>0.05).
Conclusions
Body contouring procedures are associated with improvements in QoL irrespective of the number of concurrent procedures. Further improvement in psychological well-being occurs for patients who proceed with double concurrent procedures, albeit with an increase in cost.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each submission to which Evidence-Based Medicine rankings are applicable. This excludes Review Articles, Book Reviews, and manuscripts that concern Basic Science, Animal Studies, Cadaver Studies, and Experimental Studies. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.

Similar content being viewed by others
References
Statistics. https://www.surgery.org/media/statistics. Accessed June 2 2020
Campos GM, Khoraki J, Browning MG, Pessoa BM, Mazzini GS, Wolfe L (2020) Changes in utilization of bariatric surgery in the United States from 1993 to 2016. Ann Surg 271(2):201–209. https://doi.org/10.1097/SLA.0000000000003554
Hutchison CE, Rhemtulla IA, Mauch JT et al (2019) Cutting through the fat: a retrospective analysis of clinical outcomes, cost, and quality of life with the addition of panniculectomy to ventral hernia repair in overweight patients. Hernia 23(5):969–977. https://doi.org/10.1007/s10029-019-02024-5
Simpson AM, Donato DP, Kwok AC, Agarwal JP (2019) Predictors of complications following breast reduction surgery: a national surgical quality improvement program study of 16,812 cases. J Plast Reconst Aesthet Surg 72(1):43–51. https://doi.org/10.1016/j.bjps.2018.09.002
Hutchison CE, Rhemtulla IA, Mauch JT, et al (2019) Cutting through the fat: a retrospective analysis of clinical outcomes, cost, and quality of life with the addition of panniculectomy to ventral hernia repair in overweight patients. Hernia. https://doi.org/10.1007/s10029-019-02024-5
Barone M, Cogliandro A, Salzillo R, Tambone V, Persichetti P (2018) Patient-reported satisfaction following post-bariatric surgery: a systematic review. Aesthetic Plast Surg 42(5):1320–1330. https://doi.org/10.1007/s00266-018-1146-6
Klassen AF, Kaur M, Breitkopf T, Thoma A, Cano S, Pusic A (2018) Using the BODY-Q to understand impact of weight loss, excess skin, and the need for body contouring following bariatric surgery. Plast Reconstr Surg 142(1):77–86. https://doi.org/10.1097/PRS.0000000000004461
Klassen AF, Cano SJ, Alderman A, et al. (2016) A patient-reported outcome instrument for weight loss and body contouring treatments. Plast Reconstr Surg Glob Open 4:4. doi:https://doi.org/10.1097/GOX.0000000000000665
Pierce TP, Elmallah RDK, Cherian JJ, Jauregui JJ, Mont MA (2015) Standardized questionnaire time burden for practitioners and patients. Surg Tech Int 26:302–306
BODY-Q © A Guide for Researchers and Clinicians; 2017
Shermak MA (2020) Abdominoplasty with combined surgery. Clin Plast Surg 47(3):365–377. https://doi.org/10.1016/j.cps.2020.02.001
Matarasso A, Smith DM (2015) Combined breast surgery and abdominoplasty: strategies for success. Plast Reconstr Surg 135(5):849e–860e. https://doi.org/10.1097/PRS.0000000000001238
Raghuram AC, Yu RP, Gould DJ (2020) The addition of partial or circumferential liposuction to abdominoplasty is not associated with a higher risk of skin necrosis. Aesthet Surg J. https://doi.org/10.1093/asj/sjaa251
Winocour J, Gupta V, Ramirez JR, Shack RB, Grotting JC, Higdon KK (2015) Abdominoplasty: risk factors, complication rates, and safety of combined procedures. Plast Reconstr Surg 136(5):597e–606e. https://doi.org/10.1097/PRS.0000000000001700
Saad AN, Parina R, Chang D, Gosman AA (2014) Risk of adverse outcomes when plastic surgery procedures are combined. Plast Reconstr Surg 134(6):1415–1422. https://doi.org/10.1097/PRS.0000000000000738
Bossert RP, Dreifuss S, Coon D et al (2013) Liposuction of the arm concurrent with brachioplasty in the massive weight loss patient: is it safe? Plast Reconstr Surg 131(2):357–365. https://doi.org/10.1097/PRS.0b013e3182789de9
Sozer SO, Basaran K, Alim H (2018) Abdominoplasty with circumferential liposuction: a review of 1000 consecutive cases. Plast Reconstr Surg 142(4):891–901. https://doi.org/10.1097/PRS.0000000000004819
Smith LF, Smith LF (2015) Safely combining abdominoplasty with aggressive abdominal liposuction based on perforator vessels: technique and a review of 300 consecutive cases. Plast Reconstr Surg 135(5):1357–1366. https://doi.org/10.1097/PRS.0000000000001200
Fischer JP, Tuggle CT, Wes AM, Kovach SJ (2014) Concurrent panniculectomy with open ventral hernia repair has added risk versus ventral hernia repair: an analysis of the ACS-NSQIP database. J Plast Reconstr Aesthet Surg 67(5):693–701. https://doi.org/10.1016/j.bjps.2014.01.021
Diaconu SC, McNichols CHL, AlFadil S et al (2019) Postoperative outcomes in obese patients that undergo ventral hernia repair versus ventral hernia repair with concurrent panniculectomy. Plast Reconstr Surg 143(4):1211–1219. https://doi.org/10.1097/PRS.0000000000005471
Shubinets V, Fox JP, Tecce MG et al (2017) Concurrent panniculectomy in the obese ventral hernia patient: assessment of short-term complications, hernia recurrence, and healthcare utilization. J Plast Reconstr Aesthet Surg 70(6):759–767. https://doi.org/10.1016/j.bjps.2017.01.001
Chaput B, Bertheuil N, Alet JM, Bodin F, de Bonnecaze G, Michot A (2016) Combined abdominoplasty and breast surgery versus isolated abdominoplasty: results of a systematic review. Plast Reconstr Surg 137(1):248e–249e. https://doi.org/10.1097/PRS.0000000000001919
Michot A, Alet J-M, Pélissier P, Grolleau-Raoux J-L, Bodin F, Chaput B (2016) Morbidity in combined-procedure associating abdominoplasty and breast surgery: a systematic review. Ann Chir Plast Esthet 61(1):e9–e19. https://doi.org/10.1016/j.anplas.2015.07.009
Iribarren-Moreno R, Cuenca-Pardo J, Ramos-Gallardo G (2019) Is Plastic Surgery combined with obstetrical procedures safe? Aesthetic Plast Surg 43(5):1396–1399. https://doi.org/10.1007/s00266-019-01448-9
Forte AJ, Tuggle CT, Berlin NL, Fischer JP, Persing JA (2015) Hysterectomy with concurrent panniculectomy: a propensity-matched analysis of 30-day outcomes. Plast Reconstr Surg 136(3):582–590. https://doi.org/10.1097/PRS.0000000000001535
Massenburg BB, Sanati-Mehrizy P, Ingargiola MJ, Rosa JH, Taub PJ (2015) Outcomes and Safety of the Combined Abdominoplasty-Hysterectomy: a Preliminary Study. Aesthetic Plast Surg 39(5):667–673. https://doi.org/10.1007/s00266-015-0531-7
Ali A, Essam A (2011) Abdominoplasty combined with Cesarean delivery: evaluation of the practice. Aesthetic Plast Surg 35(1):80–86. https://doi.org/10.1007/s00266-010-9563-1
Gravante G, Araco A, Sorge R et al (2008) Pulmonary embolism after combined abdominoplasty and flank liposuction: a correlation with the amount of fat removed. Ann Plast Surg. 60(6):604–608. https://doi.org/10.1097/SAP.0b013e3181344470
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. JPF has received consulting payments from Baxter, Becton-Dickinson, Gore, and Integra Life Sciences. The other authors have no financial interest to declare in relation to the content of this article. No support was received for this work.
Informed Consent
All respondents were briefed with informed consent prior to the survey.
Statement of Human Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Omar Elfanagely: Accepted for poster at the Virtual Clinical Congress 2020.
Rights and permissions
About this article
Cite this article
Elfanagely, O., Mauch, J.T., Mellia, J.A. et al. Quality of Life and Concurrent Procedures in Truncal Body Contouring Patients: A Single-Center Retrospective Study. Aesth Plast Surg 45, 1620–1627 (2021). https://doi.org/10.1007/s00266-021-02129-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-021-02129-2