Abstract
Background
Botulinum toxin treatment is the most frequently performed noninvasive cosmetic procedure performed in the USA. Because of its widespread use, an analysis of the adverse event (AE) profile of Botox injections is needed.
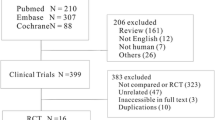
Methods
The FDA Adverse Event Report System was queried using an online web-based tool to determine the top 15 adverse events reported for four Botox brand names: Botox/Botox Cosmetic, Dysport, and Xeomin. The proportional reporting ratios (PRR) and relative odds ratios (ROR) were determined. A literature review was performed for eight AEs of clinical significance: eyelid/eyebrow ptosis, asthenia, muscular weakness, facial paresis, dysphagia, botulism, and death.
Results
Botox/Botox Cosmetic had 38367 AEs. Dysport had 3582 AEs. Xeomin had 1405 AEs. All drugs with reported cases of eyelid and eyebrow ptosis had significant PRR and ROR values. The PRR and ROR values for asthenia were not significant in any of the drugs and only reached significance for Dysport for muscular weakness and dysphagia. Both Botox/Botox Cosmetic and Dysport had elevated PRRs and RORs for facial paresis and botulism. While all drugs had at least one reported case of death related to Botox injection use, none of the PRR or ROR values were significant.
Conclusion
Known AEs for Botox injection use include eyelid/brow ptosis and muscular weakness. Feared but rare complications of Botox injection use include dysphagia, botulism, and possibly death, owing to systemic spread of the toxin. This is the first study to analyze the AE data reported to the FDA on Botox injection use.
EBM Level
III
Similar content being viewed by others
References
Surgeons, A.S.o.P.(2018) ASPS National clearinghouse of plastic surgery procedural statistics. p. 8.
Dressler D, Saberi FA (2005) Botulinum toxin: mechanisms of action. Euro Neurol 53(1):3–9
Guyuron B, Huddleston SW (1994) Aesthetic indications for botulinum toxin injection. Plast Reconstr Surg 93(5):913–918
Kao I, Drachman DB, Price DL (1976) Botulinum toxin: mechanism of presynaptic blockade. Science 193(4259):1256–1258
Sobel J (2005) Botulism. Clin Infectious Dis 41(8):1167–1173
Costa J et al. (2004) Botulinum toxin type A therapy for blepharospasm. Cochrane Database of Syst Rev (2).
Ward AB et al (2003) Use of botulinum toxin type A in management of adult spasticity-a European consensus statement. J Rehabilitation Med 35(2):98–99
Ward A et al (2004) Community management and referral of spasticity following stroke. Medendi um Gro up Publishing, Berkhamsted, UK
Molenaers G et al (2006) The effects of quantitative gait assessment and botulinum toxin a on musculoskeletal surgery in children with cerebral palsy. JBJS 88(1):161–170
Frampton JE, Easthope SE (2003) Botulinum Toxin A (Botox® Cosmetic). Am J Clin Dermatol 4(10):709–725.
Mandavia R et al (2014) The use of botulinum toxin in otorhinolaryngology: an updated review. Clin Otolaryngol 39(4):203–209
Jankovic J, Schwartz K (1990) Botulinum toxin injections for cervical dystonia. Neurology 40(2):277–277
Brin MF et al. (2009) Safety and tolerability of onabotulinumtoxinA in the treatment of facial lines: a meta-analysis of individual patient data from global clinical registration studies in 1678 participants. J Am Acad Dermatol 61(6):961–70.e1–11.
Naumann M, Jankovic J (2004) Safety of botulinum toxin type A: a systematic review and meta-analysis. Curr Med Res Opin 20(7):981–990
Cavallini M et al (2014) Safety of botulinum toxin A in aesthetic treatments: a systematic review of clinical studies. Dermatol Surg 40(5):525–536
Coté TR et al (2005) Botulinum toxin type A injections: adverse events reported to the US Food and Drug Administration in therapeutic and cosmetic cases. J Am Acad Dermatol 53(3):407–415
Ault A (2008) New Botulinum Toxin injection warnings issued postinjection symptoms include dysphagia, ptosis, and shortness of breath, according to the FDA. Skin Allergy News 39(3):13–13
Dashtipour K, Pedouim F (2016) Botulinum Toxin: preparations for clinical use, immunogenicity, side effects, and safety profile. Semin Neurol 36(1):29–33
Klein AW (2004) Contraindications and complications with the use of botulinum toxin. Clin Dermatol 22(1):66–75
Yiannakopoulou E (2015) Serious and long-term adverse events associated with the therapeutic and cosmetic use of botulinum toxin. Pharmacology 95(1–2):65–69
Nong LB et al (2008) Severe respiratory failure after injection of botulinum toxin: case report and review of the literature. Zhonghua Jie He He Hu Xi Za Zhi 31(5):369–371
Tugnoli V et al (2002) Botulism-like syndrome after botulinum toxin type A injections for focal hyperhidrosis. Br J Dermatol 147(4):808–809
Administration, U.S.F.D. Questions and Answers on FDA’s Adverse Event Reporting System (FAERS). [cited 2019 November 27]; Available from: https://www.fda.gov/drugs/surveillance/questions-and-answers-fdas-adverse-event-reporting-system-faers.
TLIBRXZ K-h (2015) Open FDA: Proportional Reporting Ratio (PRR) for a drug. [cited 2020 January 3]; Available from: https://openfda.shinyapps.io/RR_D/.
Bate A, Edwards I (2006) Data mining in spontaneous reports. Basic Clin Pharmacol Toxicol 2006. 98(3):324–330.
Almenoff JS et al (2006) Comparative performance of two quantitative safety signalling methods. Drug Saf 29(10):875–887
Evans SJ, Waller PC, Davis S (2001) Use of proportional reporting ratios (PRRs) for signal generation from spontaneous adverse drug reaction reports. Pharmacoepidemiol Drug Safety 10(6):483–486
Sakaeda T et al (2013) Data mining of the public version of the FDA Adverse Event Reporting System. Int J Med Sci 10(7):796
Böhm R. Primer on disproportionality analysis. Version: 2018-10-16. http://openvigil.sourceforge.net/doc/DPA.pdf
(EV-EWG), E.M.A.E.E.W.G. (2006)Guideline on the Use of statistical signal detection methods in the Eudravigilance data analysis system. Evaluation of medicines for human use, November 16.
Bate A et al (1998) A Bayesian neural network method for adverse drug reaction signal generation. Euro J Clin Pharmacol 54(4):315–321
Walker TJ, Dayan SH (2014) Comparison and overview of currently available neurotoxins. J Clin Aesthetic Dermatol 7(2):31
Cox SE, Adigun CG (2011) Complications of injectable fillers and neurotoxins. Dermatol Ther 24(6):524–536.
Filipo R et al (2012) Botulinum toxin in the treatment of facial synkinesis and hyperkinesis. Laryngoscope 122(2):266–270
de Maio M, Bento RF (2007) Botulinum toxin in facial palsy: an effective treatment for contralateral hyperkinesis. Plast Reconstr Surg 20(4):917–927; discussion 928.
Trindade de Almeida AR, Secco LC, Carruthers A (2011) Handling botulinum toxins: an updated literature review. Dermatol Surg 37(11):1553–1565
Sundaram H et al (2016) Global aesthetics consensus: hyaluronic acid fillers and Botulinum Toxin Type A-recommendations for combined treatment and optimizing outcomes in diverse patient populations. Plast Reconstr Surg 137(5):1410–1423
Carruthers A, Carruthers J (2005) Botulinum toxin type A. J Am Acad Dermatol 53(2):284–290
Sundaram H et al (2016) Aesthetic applications of botulinum toxin A in Asians: an international, multidisciplinary, Pan-Asian consensus. Plastic Reconstructive Surg Global Open 4(12).
Ferrari A et al (2018) Pharmacological differences and clinical implications of various botulinum toxin preparations: a critical appraisal. Funct Neurol 33(1):7
Simpson DM et al (2016) Practice guideline update summary: Botulinum neurotoxin for the treatment of blepharospasm, cervical dystonia, adult spasticity, and headache: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology 86(19):1818–1826
Aoki K et al (2005) Pharmacology of Botox, Dysport, Myobloc and BTX-A in animal models of efficacy and safety. In: Abstract presented at the international conference on basic and therapeutic aspects of Botulinum and Tetanus Toxins, Denver.
Aoki KR (2002) Botulinum neurotoxin serotypes A and B preparations have different safety margins in preclinical models of muscle weakening efficacy and systemic safety. Toxicon 40(7):923–928
Ranoux D et al (2002) Respective potencies of Botox and Dysport: a double blind, randomised, crossover study in cervical dystonia. J Neurol Neurosurg Psychiatry 72(4):459–462
Adams G, Kirkness C, Lee J (1987) Botulinum toxin A induced protective ptosis. Eye 1(5):603–608
Kirkness CM et al (1988) Botulinum toxin A-induced protective ptosis in corneal disease. Ophthalmology 95(4):473–480
Jankovic J, Brin MF (1991) Therapeutic uses of botulinum toxin. New England J Med 324(17):1186–1194
Ellis MF, Daniell M (2001) An evaluation of the safety and efficacy of botulinum toxin type A (BOTOX) when used to produce a protective ptosis. Clin Exp Ophthalmol 29(6):394–399
Naik M et al (2008) Anterior chemodenervation of levator palpebrae superioris with botulinum toxin type-A (Botox®) to induce temporary ptosis for corneal protection. Eye 22(9):1132–1136
Reddy UP, Woodward JA (2010) Abobotulinum toxin A (Dysport) and botulinum toxin type A (Botox) for purposeful induction of eyelid ptosis. Ophthal PlastReconstr Surg 26(6):489–491
Ward SR, Minamoto VB, Suzuki KP, Hulst JB, Bremner SN, Lieber RL (2018) Recovery of rat muscle size but not function more than 1 year after a single botulinum toxin injection. Muscle Nerve 57(3):435–441
Matharu MS BOTOX®(Botulinum toxin type A, BoNTA, Allergan) in the management of chronic migraine.
Yaraskavitch M, Leonard T, Herzog W (2008) Botox produces functional weakness in non-injected muscles adjacent to the target muscle. J Biomech 41(4):897–902
Carruthers JA et al (2002) A multicenter, double-blind, randomized, placebo-controlled study of the efficacy and safety of botulinum toxin type A in the treatment of glabellar lines. J Am Acad Dermatol 46(6):840–849
Salles AG, Toledo PN, Ferreira MC (2009) Botulinum toxin injection in long-standing facial paralysis patients: improvement of facial symmetry observed up to 6 months. Aesthetic Plastic Surg 33(4):582–590
Kim J (2013) Contralateral botulinum toxin injection to improve facial asymmetry after acute facial paralysis. Otol Neurotol 34(2):319–324
Mehdizadeh OB, Dielsn J, White MW (2016) Botulinum toxin in the treatment of facial paralysis. Facial Plastic Surg Clin 24(1):11–20.
Roggenkämper P et al (1994) Orbicular synkinesis after facial paralysis: treatment with botulinum toxin. Doc Ophthalmol 86(4):395–402
Omprakash H, Rajendran S (2008) Botulinum toxin deaths: What is the fact? J Cutaneous Aesthetic Surg 1(2):95
Bhatia KP et al (1999) Generalised muscular weakness after botulinum toxin injections for dystonia: a report of three cases. J Neurol Neurosurg Psychiatry 67(1):90–93
Wilson F (2001) Botulinum toxin-A risks overcome by proper technique. Cosmetic Surg Times 12.
Comella CL, Tanner CM, DeFoor-Hill L, Smith C (1992) Dysphagia after botulinum toxin injections for spasmodic torticollis: clinical and radiologic findings. Neurology 42(7):1307–1310. https://doi.org/10.1212/wnl.42.7.1307
Zaninotto G et al (2004) The role of botulinum toxin injection and upper esophageal sphincter myotomy in treating oropharyngeal dysphagia. J Gastrointestinal Surg 8(8):997–1006
Pasricha PJ et al (1994) Treatment of achalasia with intrasphincteric injection of botulinum toxin: a pilot trial. Ann Internal Med 121(8):590–591
Mya NK et al (2019) Botox: the deadly beauty. Forensic Med Anat Res 7(1):13–17
Li M, Goldberger BA, Hopkins C (2005) Fatal case of BOTOX®-related anaphylaxis? J Forensic Sci 50(1):JFS2004196-4.
Rosenfield LK et al (2014) The first case report of a systemic allergy to onabotulinumtoxinA (Botox) in a healthy patient. Aesthetic Surg J 34(5):766–768
Funding
NA
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest to disclose.
Statement of human and animal rights or ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ahsanuddin, S., Roy, S., Nasser, W. et al. Adverse Events Associated With Botox as Reported in a Food and Drug Administration Database. Aesth Plast Surg 45, 1201–1209 (2021). https://doi.org/10.1007/s00266-020-02027-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-020-02027-z