Abstract
Background
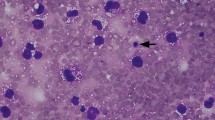
First described in 1997, breast implant-associated anaplastic large cell lymphoma (BIA-ALCL) was recognised by the World Health Organisation in 2016 as a specific disease. It typically presents as a late seromacontaining atypical, monoclonal T cells which are CD30+ and anaplastic lymphoma kinase negative. Until recently, it was thought that the disease was very rare. However, it is being diagnosed increasingly frequently with 56 cases confirmed in Australia by September 2017 and the estimated incidence revised from 1 in 300,000 to between 1 in 1000 and 1 in 10,000 patients with bilateral implants. There is debate about the spectrum of BIA-ALCL. According to the current WHO classification, BIA-ALCL is a cancer in all cases. Treatment guidelines require that it is treated urgently with a minimum of bilateral removal of implants and capsulectomies. Whilst acknowledging the disease has been under diagnosed in the past, with some notable exceptions the BIA-ALCL literature has given scant attention to the epidemiological evidence. Now that it is known that the disease may occur in up to 1 in 1000 patients with a median of 7.5 years from implantation to diagnosis, understanding it in its epidemiological context is imperative. The epidemiology of cancer and lymphoma in women with breast implants strongly suggests that most patients do not have a cancer that will inevitably progress without treatment but instead a self-limiting lympho-proliferative disorder. Although the possibility of spontaneous regression has been raised and the observation made that treatment delay did not seem to increase the risk of spread, the main objection to the lympho-proliferative hypothesis has been the lack of documented cases of spontaneous regression or resolution. Because all cases currently are considered malignant and treated urgently, only case report evidence, interpreted in the proper epidemiological context, is likely to be available to challenge this thinking.
Methods and Results
New observations and interpretation of the epidemiology of BIA-ALCL are made. These are supported by the presentation of two cases, which to the best of our knowledge comprise the first documented evidence of spontaneous regression and spontaneous resolution of confirmed BIA-ALCL.
Conclusions
The epidemiology of the disease strongly suggests that the vast majority of cases are not a cancer that will inevitably progress without treatment. The findings presented in the manuscript provide supportive clinical evidence. Consequently, an alternative view of BIA-ALCL with implications for research, diagnosis and clinical management needs to be considered.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
References
Keech Jr., J.A., Creech, B.J.: Anaplastic T-cell lymphoma in proximity to a saline-filled breast implant. Plast Reconstr Surg 100(2), 554–555 (1997)
Swerdlow, S.H., Campo, E., Pileri, S.A., et al.: The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood 127(20), 2375–2390 (2016)
Anaplastic large cell lymphoma (ALCL) in women with breast implants: preliminary FDA findings and analyses. In: Services DoHaH (ed). US Food and Drug Administration, Washington, DC (2013)
Breast implants and anaplastic large cell lymphoma. Update-additional confirmed cases of anaplastic large cell lymphoma (2017). https://www.tga.gov.au/alert/breast-implants-and-anaplastic-largecell-lymphoma. Accessed 4 Dec 2017
Breast implants and anaplastic large cell lymphoma. Expert advisory panel advice on association with anaplastic large cell lymphoma (2016). https://www.tga.gov.au/alert/breast-implants. Accessed 26 Dec 2016
Story, S.K., Schowalter, M.K., Geskin, L.J.: Breast implantassociated ALCL: a unique entity in the spectrum of CD30? lymphoproliferative disorders. Oncologist 18(3), 301–307 (2013)
Miranda, R.N., Aladily, T.N., Prince, H.M., et al.: Breast implantassociated anaplastic large-cell lymphoma: long-term follow-up of 60 patients. J Clin Oncol 32(2), 114–120 (2014)
Clemens, M.W., Medeiros, L.J., Butler, C.E., et al.: Complete surgical excision is essential for the management of patients with breast implant-associated anaplastic large-cell lymphoma. J Clin Oncol 34(2), 160–168 (2016)
Brody, G.S., Deapen, D., Taylor, C.R., et al.: Anaplastic large cell lymphoma occurring in women with breast implants: analysis of 173 cases. Plast Reconstr Surg 135(3), 695–705 (2015)
Rupani, A., Frame, J.D., Kamel, D.: Lymphomas associated with breast implants: a review of the literature. Aesthet Surg J 35(5), 533–544 (2015)
Loch-Wilkinson, A., Beath, K.J., Knight, R.J.W., et al.: Breast implant-associated anaplastic large cell lymphoma in Australia and New Zealand: high-surface-area textured implants are associated with increased risk. Plast Reconstr Surg 140(4), 645–654 (2017)
Brinton, L.A., Lubin, J.H., Burich, M.C., Colton, T., Brown, S.L., Hoover, R.N.: Cancer risk at sites other than the breast following augmentation mammoplasty. Ann Epidemiol 11(4), 248–256 (2001)
Brisson, J., Holowaty, E.J., Villeneuve, P.J., et al.: Cancer incidence in a cohort of Ontario and Quebec women having bilateral breast augmentation. Int J Cancer 118(11), 2854–2862 (2006)
Laurent, C., Delas, A., Gaulard, P., et al.: Breast implant-associated anaplastic large cell lymphoma: two distinct clinicopathological variants with different outcomes. Ann Oncol 27(2), 306–314 (2016)
Lipworth, L., Tarone, R.E., Friis, S., et al.: Cancer among Scandinavian women with cosmetic breast implants: a pooled long-term follow-up study. Int J Cancer 124(2), 490–493 (2009)
Lipworth, L., Tarone, R.E., McLaughlin, J.K.: Breast implants and lymphoma risk: a review of the epidemiologic evidence through 2008. Plast Reconstr Surg 123(3), 790–793 (2009)
Vase, M.O., Friis, S., Bautz, A., Bendix, K., Sorensen, H.T., d'Amore, F.: Breast implants and anaplastic large-cell lymphoma: a Danish population-based cohort study. Cancer Epidemiol Biomark Prev 22(11), 2126–2129 (2013)
Agrawal, B., Reddish, M., Longenecker, B.M.: CD30 expression on human CD8? T cells isolated from peripheral blood lymphocytes of normal donors. J Immunol 157(8), 3229–3234 (1996)
Tarkowski, M.: Expression and function of CD30 on T lymphocytes. Arch Immunol Ther Exp (Warsz) 47(4), 217–221 (1999)
Kadin, M., Morgan, J., Xu, H., Glicksman, C.A.: CD30? T cells in late seroma may not be diagnostic of breast implant-associated anaplastic large cell lymphoma. Aesthet Surg J 37(7), 771–775 (2017)
Deva AK (2017) Personal communication to corresponding author
Hart, A.M., Lechowicz, M.J., Peters, K.K., Holden, J., Carlson, G.W.: Breast implant-associated anaplastic large cell lymphoma: report of 2 cases and review of the literature. Aesthet Surg J. 34(6), 884–894 (2014)
Australian Institute of Health and Welfare 2017. Cancer in Australia 2017. Cancer series no.101.Cat. no. CAN 100. AIHW, Canberra
Park, B.Y., Lee, D.H., Lim, S.Y., et al.: Is late seroma a phenomenon related to textured implants? A report of rare complications and a literature review. Aesthet Plast Surg 38(1), 139–145 (2014)
Spear, S.L., Rottman, S.J., Glicksman, C., Brown, M., Al-Attar, A.: Late seromas after breast implants: theory and practice. Plast Reconstr Surg 130(2), 423–435 (2012)
Park, S., Oh, C.M., Cho, H., et al.: Association between screening and the thyroid cancer "epidemic" in South Korea: evidence from a nationwide study. BMJ 355, i5745 (2016)
Macaulay WL (1968) Lymphomatoid papulosis. A continuing self-healing eruption, clinically benign–histologically malignant. Arch Dermatol 97(1):23–30
Kadin, M.E., Xu, H., Pavlov, I.: Breast implant associated ALCL closely resembles primary cutaneous ALCL. Lab Invest 92(Suppl 1), 346A (2012)
Kempf, W., Pfaltz, K., Vermeer, M.H., et al.: EORTC, ISCL, and USCLC consensus recommendations for the treatment of primary cutaneous CD30-positive lymphoproliferative disorders: lymphomatoid papulosis and primary cutaneous anaplastic largecell lymphoma. Blood 118(15), 4024–4035 (2011)
Sieber, D.A., Adams Jr., W.P.: What's your micromort? A patient-oriented analysis of breast implant-associated anaplastic large cell lymphoma (BIA-ALCL). Aesthet Surg J 37(8), 887–891 (2017)
Esserman, L.J., Thompson, I.M., Reid, B., et al.: Addressing overdiagnosis and overtreatment in cancer: a prescription for change. Lancet Oncol 15(6), e234–e242 (2014)
Woods, W.G., Gao, R.N., Shuster, J.J., et al.: Screening of infants and mortality due to neuroblastoma. N Engl J Med 346(14), 1041–1046 (2002)
Acknowledgements
The authors wish to thank Dr. Roberto Miranda at the MD Anderson Cancer Centre, for his review of the slides of both cases, and Dr. Linda Shen at Pathology Queensland, for her assistance with the case of spontaneous resolution.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The first author has previously acted as a consultant to the Silimed Corporation. All other authors have no conflicts of interest to disclose.
Additional information
This article is being reprinted for ISAPS 50th Anniversary Special Issue.
Rights and permissions
About this article
Cite this article
Fleming, D., Stone, J. & Tansley, P. Spontaneous Regression and Resolution of Breast Implant-Associated Anaplastic Large Cell Lymphoma: Implications for Research, Diagnosis and Clinical Management. Aesth Plast Surg 44, 1109–1115 (2020). https://doi.org/10.1007/s00266-020-01810-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-020-01810-2