Abstract
Introduction
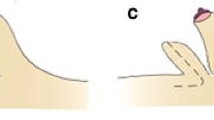
Tuberous breast deformity, even rarely, might be observed in the gynecomastia population. It can clinically appear very similar to tuberous breast in females, including a footprint resembling a feminine inframammary fold (IMF). Because of its anatomical characteristics, its correction could benefit from particular surgical measures and therefore it should be careful diagnosed. A clear footprint defining a very feminine inframammary fold is very difficult to correct and renders very difficult the management of the extra skin. Transection of the fibrous constrictions at the level of inframammary fold is not sufficient to obtain a satisfactory result, and adjunctive surgical measurements are required.
Materials and Methods
From January 2007 to December 2015, twenty-one patients, affected by gynecomastia with tuberous breast deformity, underwent surgical correction consisting of parenchyma debulking and transection of the stenotic fibrous ring of the footprint. The recontouring of the chest profile was optimized using parenchymal flaps which helped to maximize the surgical correction with minimal scarring.
Result
The mean age at surgery was 28.8 years. The average follow-up period was 32 months. The average hospitalization stay was 1.28 days. Routine laboratory tests and histological examinations did not demonstrate any anomalies. No major complications and no recurrences of the disorders have not been observed. No major complications were reported: one seroma, one skin depression, two scar revisions and three cases of bilateral minimal crescent ptotic skin appearance were observed.
Conclusion
Although tuberous breast in the gynecomastia population is a rare clinical entity, it should be taken into consideration because it could benefit from some specific surgical measures. The use of glandular flaps showed a satisfactory reshaping of the pectoral area.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.





Similar content being viewed by others
References
Rohrich R, Ha R, Kenkel J Jr (2003) Adams WP Classification and management of gynecomastia: defining the role of ultrasound- assisted liposuction. Plast Recon Surg 111(2):909–923
Innocenti A, Innocenti M, Mori F et al. (2017) Tuberous breast, past present and future: personal classification treatment and surgical outcomes. Ann Plast Surg 80(2):104–108
Lazala C, Saenger P (2002) Pubertal gynecomastia. J Pediatr Endocrinol Metab 15:553–560
Pacifico MD, Kang NV (2007) The tuberous breast revisited. J Plast Reconstr Aesthet Surg 60:455–464
Innocenti A, Innocenti M (2015) Retro-areola distally based flap in the management of the full expression of tuberous breast: a simple strategy to resolve a weak point of the deformity. Aesth Plast Surg 39(5):700–705
Innocenti A, Melita D, Ghezzi S, Ciancio F (2018) stenotic breast malformation and its reconstructive surgical correction: a new concept from minor deformity to tuberous breast. Aesth Plast Surg 42(3):911–912
Portincasa A, Ciancio F, Cagiano L, Innocenti A, Parisi D (2017) Septum-enhanced mammaplasty in inferocentral pedicled breast reduction of macromastia and gigantomastia patients. Aesth Plast Surg 41(5):1037–1044
Aiache AE (1989) Surgical treatment of gynecomastia in the bodybuilder. Plast Reconstr Surg 83:61–66
Webster JP (1946) Mastectomy for gynecomastia through a semicircular-intra-areolar incision. Ann Surg 124:557–575
Grolleau J, Lanfrey E, Lavigne B et al (1999) Breast base anomalies: treatment strategy for tuberous breasts, minor deformities, and asymmetry. Plast Reconstr Surg 104:2040–2048
Ridha H et al (2009) How happy are patients with their gynaecomastia reduction surgery? J Plast Reconstr Aesthet Surg 62(11):1473–1478
Innocenti A, Andretto AC, Ciancio F (2014) Wide-undermining neck liposuction: tips and trick for good results. Aesth Plast Surg. 38(4):662–669
Rees T, Aston S (1976) The tuberous breast. Clin Plast Surg 3:339–347
Pacifico M, Kang NV (2007) The tuberous breast revisited. J Plast Reconstr Aesthet Surg 60:455–464
Mandrekas A, Zambacos G, Anastasopoulos A et al (2003) Aesthetic reconstruction of the tuberous breast deformity. Plast Reconstr Surg 12:1099–1180
Hamilton S, Gault D (2003) The tuberous male breast. Br J Plast Surg 56(3):295–300
Klinger M, Caviggioli F, Klinger F, Villani F, Arra E, Di Tommaso (2011) Tuberous breast: morphological study and overview of a borderline entity. Can J Plast Surg 19(2):42–44
Godwin Y (2018) Correction of tuberous nipple areolar complex deformity in gynecomastia: the deformity that can get forgotten. Ann Plast Surg. 81(1):3–6
Huang T, Hidalgo J, Lewis S (1982) A circumareolar approach in surgical management of gynecomastia. Plast Reconstr Surg 69:35–40
Reyes R, Zicchi S, Hamed H, Chaudary M, Fentiman I (1995) Surgical correction of gynaecomastia in bodybuilders. Br J Clin Pract 49:177–179
Mordcai B, Ron H (2015) Correction of Gynecomastia in body builders and patients with good physique. Plast Reconstr Surg 135(2):425–432
Innocenti A, Ciancio F, Mori F, Melita D, Innocenti M (2017) Comment to: No-drain single incision liposuction pull-through technique for gynecomastia. Aesth Plast Surg 41(4):990–991
Innocenti A, Melita D, Mori F, Ciancio F, Innocenti M (2017) Comment to “Postero-Inferior pedicle surgical technique for the treatment of grade III Gynecomastia”. Aesth Plast Surg 41:747–748
Innocenti A, Ciancio F, Portincasa A, Parisi D (2017) Discussion: Surgical management of gynecomastia-subcutaneous mastectomy and liposuction. Aesth Plast Surg 41(4):983–984
Innocenti A, Melita M, Ciancio F, Innocenti M (2017) Discussion: long-term follow-up of recurrence and patient satisfaction after treatment of gynecomastia. Aesth Plast Surg. 41(5):1242–1243
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Innocenti, A. Male Tuberous Breast: A Rare Variant of Gynecomastia. Clinical Considerations and Personal Experience: Tips and Tricks to Maximize Surgical Outcomes. Aesth Plast Surg 43, 1500–1505 (2019). https://doi.org/10.1007/s00266-019-01418-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-019-01418-1