Abstract
Introduction
Neovaginal atresia especially following male-to-female transgender vaginoplasty is a distressing concern. A pelvic space must be re-created. Traditionally, an epithelial or mucosal lining is employed to cover the space. However, in our series of 18 patients, a non-grafted approach has been equally efficacious, as previously described by others.
Aim
To follow the outcome of male-to-female transsexuals undergoing secondary depth enhancement without use of graft or flap.
Methods
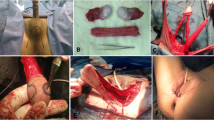
Patient selection included two operated on elsewhere, one of whom had a lower abdominal skin graft, and the remainder done here using an inverted penile skin flap supplemented by a scrotal graft extension as needed. The time lag from primary to revision surgery varied from 5 months to 23 years, average 3.7 years. The fascial plane of Denonvilliers was reopened and packed for 7 days to facilitate maintenance of a pelvic space. Patients are requested to perform serial self-dilations with a stent set indefinitely to maintain patency and procure additional depth. Immuno-histochemistry staining was performed to demonstrate estrogen receptor (ER) presence in male genital skin. Estrogen cream may be utilized to facilitate wound healing. Main outcome measures were post-operative depth results and Female Sexual Function Index (FSFI) scores. Several attempts were made to contact all patients for completion of a FSFI. Ten out of 18 responded.
Results
Following revision of the pelvic space, static depths increased two-fold on average, from 2.4 in. (6.2 cm) to 5.0 in. (12.7 cm). The FSFI domain scores (of desire, arousal, lubrication, orgasm, satisfaction, and pain) were all mid-range or above. Full scale FSFI scores (compilation score) averaged 23.4 (range limits 2–36). Histologic staining showed the presence of ER in genital skin of all genetic males tested regardless of estrogen usage and perceived gender.
Conclusions
Given adequate development of the rectal-vesical space and preservation of that space with self-dilation, epithelialization will ensue providing sexual gratification for patient and partner (as per patient).
Level of Evidence III
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.





Similar content being viewed by others
References
Dupuytren M (1827) Quatri ~ me revue chirurgicale de l’Hotel-Dieu. La Clinique des Hôpitaux et de la Ville 35:1–3
Abbe R (1898) New method of creating a vagina in a case of congenital absence. NY Meds Rec 54:836–838
McIndoe AH, Banister JB (1938) An operation for the cure of congenital absence of the vagina. J Obstet Gynaecol Br Commonw 45:490–494
Wharton R (1938) A simple method of constructing a vagina. Ann Surg 107:842–854
Counseller VS, Flor FS (1957) Congenital absence of the vagina: further results of treatment and a new technique. Surg Clin North Am 37(1107–18):2
McQuillan SK, Grover SR (2013) Dilation and surgical management in vaginal agenesis: a systematic review. Int Urogynecol J 25:2219–2221
Michala L, Strawbridge L, Bikoo M, Cutner AS, Creighton SM (2013) Lower urinary tract symptoms in women with vaginal agenesis. Int Urogynecol J 24:425–429
Bianchi S, Frontino G, Ciappina N, Restelli R (2011) Fedele L creation of neovagina in Rokitansky syndrome: comparison between two laparoscopic techniques. Fertil Steril 95:1098–1100
Androgen insensitivity support group (2013). Vaginal hypospadiac from www.aissg.org/31_hplasia.htm<http://www.aissg.org/31_hplasia.htm> May, 2013
Alessandrescu D, Peltecu GC, Buhimschi CS, Buhimschi IA (1996) Neocolpopoiesis with split-thickness skin graft as a surgical treatment of vaginal agenesis: retrospective review of 201 cases. Am J Obstet Gynecol 175:131–136
Small MP (1987) Penile and scrotal inversion vaginoplasty for male to female transsexuals. Urology 29:593–597
Killick SR, Leary C, Trussell J, Guthrie KA (2011) Sperm content of pre-ejaculatory fluid. Human Fertil 14(1):48–52
Mobus V, Sachweh K, Knapstein PG, Kreienberg R (1993) Women after surgically corrected vaginal aplasia a followup of psychosexual rehabilitation. Geburtshilfe Frauenheilk 53:125–131
Borruto F, Camoglio FS, Zampieri N, Fedele L (2007) The laparoscopic Vecchietti technique for vaginal agenesis. Intern J Gynecol Obstet 98:15–19
Csermely T, Halvax L, Sarkany A, Jeges S, Vizer M, Bozsa S, Farkas B, Bodis J (2011) Sexual function after modified laparoscopic Vecchietti’s vaginoplasty. J Pediatrc Adoles Gynecol 24:147–152
Frank RTO (1938) The formation of an artificial vagina without operation. Am J Obstet Gynecol 35:1053–1055
Ingram M (1981) The bicycle seat stool in the treatment of vaginal agenesis and stenosis: a preliminary report. Am J Obstet Gynecol 140:867–873
Creatsas G, Deligeoroglou E (2010) Creatsas modification of Williams vaginoplasty for reconstruction of the vaginal aplasia in Mayer–Rokitansky–Kuster–Hauser syndrome cases. Women’s Health 6:367–375
Lee M-H (2006) Non-surgical treatment of vaginal agenesis using a simplified version of Ingram’s method. Yonsei Med J 47:892–895
Roberts CP, Haber MJ, Rock JA (2001) Vaginal creation for Mullerian agenesis. Am J Obstet Gynecol 185:1349–1352
Borruto F, Chasen ST, Chervenak FA, Fedele L (1999) The Vecchietti procedure for the surgical treatment of vaginal agenesis: comparison of laparoscopy and laparotomy. Int J Gynecol Obstet 64:153–158
Gauwerky JFH, Wallwiener D, Bastert G (1992) An endoscopically assisted technique for construction of neovagina. Arch Gynecol Obstet 252:59–63
Brucker SY, Gegusch M, Zubke W, Rall K, Gauwerky JF, Wallwiener D (2008) Neovagina creation in vaginal agenesis: development of a new laparoscopic Vecchietti-based procedure and optimized instruments in a prospective comparative interventional study in 101 patients. Fertil Steril 90:1940–1952
Chatwani A, Nyirjesy P, Harmanli OH, Grody MHT (1999) Creation of Neovagina by laparoscopic Vecchietti operation. J Laparoendosc Adv Surg Tech 9:425–427
Harmanli OH, Grody MHT (2008) Laparoscopic Vecchietti procedure: improving on an indispensable method. Am J Obstet Gynecol 199:713.e1-2
Popp LW, Ghirardini G (1992) Creation of neovagina by pelviscopy. J Laparoendosc Surg 2:165–173
Fedele L, Busacca M, Candiani M, Vignali M (1994) Laparoscopic creation of a neovagina in Mayer-Rokitansky-Küster-Hauser syndrome by modification of Vecchietti’s operation. Am J Obstet Gynecol 197:209–268
Fedele L, Bianchi S, Frontino G, Ciappina G, Fontana E, Borruto F (2007) Laparoscopic findings and pelvic anatomy in Mayer–Rokitansky–Küster–Hauser syndrome. Obstet Gynecol 109:1111–1115
Keckstein C, Buck C, Sasse V, Tuttlies F, Ulrich U (1995) Laparoscopic creation of a neovagina: Modified Vecchietti method. End Surg 3:93–95
Oliveira MAP, Kano AEU, Melki LAH, Lasmar RB, de Oliveira HC (2008) A simple and effective traction device for laparoscopic formation of a neovagina using the Vecchietti technique. J Minim Invasive Gynecol 15:611–614
Csermely T, Halvax L, Vizer M, Tamas P, Kovacs K, Gocze P, Szabo I, Szilagyi A (2007) The application of ‘endovaginal’ sonography during a laparoscopy-assisted Vecchetti operation. Acta Obstet et Gynecol 86:1231–1235
Fedele L, Bianchi S, Frontino G, Fontana E, Restelli E, Bruni Z (2008) The laparoscopic Vecchietti’s modified technique in Rokatansky syndrome: anatomic, functional, and sexual long-term results. Am J Obstet Gynecol 377:e1–e6
Bianchi M, Sola V, Ricci P, Pomes C (2007) Late post-operative urinary stress incontinence after a laparoscopic-assisted Vecchietti procedure for neovagina creation in a patient with Rokitansky syndrome: successful treatment with the TVT-O technique. J Minim Invasive Gynecol 14:116–118
Abramowicz S, Oden S, Joutel N, Roman A, Gromez A, Marpeau L (2013) Laparoscopic creation of a neovagina by Vecchietti’s technique: anatomic and functional results. Gynecol Obstet Fertil 41(41):4–9
Rouzi AA (2013) Urethral sex in a woman with previously undiagnosed Mayer–Rokitansky–Küster–Hauser syndrome. Clin Exp Obstet Gynecol 40:452–453
Davydov SN, Zhvitiashvili OD (1974) Formation of vagina (colpopoiesis) from peritoneum of Douglas pouch. Acta Chir Plast 16:35–40
Ismail IS, Cuter AS, Creighton SM (2006) Laparoscopic vaginoplasty: alternative technique in vaginal reconstruction. B JOG 113:340–343
Baldwin JF (1904) The formation of an artificial vagina by intestinal transplantation. Ann Surg 40:398
Liguori G, Trombetta C, Bucci S, Salame L, Bortul S, Siracusano S, Belgrano E (2005) Laparoscopic mobilization of neovagina to assist secondary ileal vaginoplasty in male-to-female transsexuals. Urology 66:293–298
Burger RA, Riedmiller H, Knapstein PG, Friedberg V, Hohenfellner R (1989) Ileocecal vaginal construction. Am J Obstet Gynecol 161:162–167
Wesley JR, Coran AG (1992) Intestinal vaginoplasty for congenital absence of the vagina. J Pediatr Surg 27:885–889
Franz RC (1996) Sigmoid colon vaginoplasty: a modified method. Br J Obstet Gynecol 103:1148–1155
Lenaghan R, Wilson N, Lucas CE, Ledgerwood AM (1997) The role of rectosigmoid neocolporrhaphy. Surgery. 122:856–860
Hensle TW, Riley EA (1998) Vaginal replacement in children and young adults. J Urol 159:1035–1038
Lima M, Ruggeri G, Randi B, Domini M, Gargano T, La Pergola E, Gregori G (2010) Vaginal replacement in the pediatric age group: a 34-year experience of intestinal vaginoplasty in children and young girls. J Pediatr Surg 45:2087–2091
Djordjevic ML, Stanojevic DS, Bizic MR (2011) Rectosigmoid vaginoplasty: clinical experience and outcome in 88 cases. J Sex Med 8:3487–3494
Edmonds DK (2003) Congenital malformation of the genital tract and their management. Best Pract Res Clin Obstet Gynecol 17:19–40
Franz RC (1996) Sigmoid colon vaginoplasty: a modified method. Br J Obstet Gynecol 103:1148–1155
Williams EA (1964) Congenital absence of the vagina. A simple operation for its relief. J Obstet Gynaecol Br Commonw 71:511–516
Williams EA (1970) Vulva-vaginoplasty. Proc Roy Soc Med 63:40
South G (1985) Nursing care study. Williams vaginoplasty. Nurs Mirror. 160:46–50
Feroze RM, Demurest CJ, Welply G (1975) Vaginoplasty at the Chelsea Hospital for women: a comparison of two techniques. Br J Obstet Gynecol 82:536–540
Jackson ND (1994) Rosettblat PL use of interceed absorbable adhesion barrier for vaginoplasty. Obstet Gynecol 84:1048–1050
Buss JG, Lee RA (1989) McIndoe procedure for vaginal agenesis: results and complications. Mayo Clin Proc 64:758–761
Ozek C, Gurler T, Alper M, Gundogan H, Bilkay U, Songur E, Akin Y, Cagdas A (1999) Modified McIndoe procedures for vaginal agenesis. Ann Plast Surg 43:393–396
Hage JJ, Karim RB (1998) Abdominoplastic secondary full-thickness skin graft vaginoplasty for male-to-female transsexuals. Plast Reconstr Surg 101:1512–1515
Saraf S, Saraf P (2006) McIndoe vaginoplasty: revisited. Internet J Gynecol Obstet 6:1–12
Ashworth MF, Morton KE, Dewhurst J, Lilford RJ, Bates RG (1986) Vaginoplasty using amnion. Obstet Gynecol 67:443–446
Nisolle M, Donnez J (1992) Vaginoplasty using amniotic membranes in cases of vaginal agenesis or after vaginectomy. J Gynecol Surg 8:25–30
Zafar M, Saeed S, Kant B, Murtaza B, Dar MF, Khan NA (2007) Use of amnion in vaginoplasty for vaginal atresia. J Coll Phys Surg Pak 17:107–109
Lin W, Chang C, Shen YY, Tsai H (2003) Use of autologous buccal mucosa for vaginoplasty: a study of 8 cases. Hum Reprod 18:604
Oakes MB, Beck S, Smith YB, Quint EH, Park JM (2010) Augmentation vaginoplasty of colonic neovagina stricture using oral mucosa graft. J Pediatr Adolesc Gynecol 23:e39–e342
Ozgenel GY, Ozcan M (2003) Neovaginal construction with buccal mucosa grafts. Plast Reconstr Surg 111:2250–2254
Soong YK, Chang FH, Lai YM, Lee CL, Chou HH (1996) Results of laparoscopically assisted neovaginoplasty in 18 patients with congenital absence of the vagina. Hum Reprod 11:200–203
Martinez-Mora J, Isnard R, Castellvi IR (1992) Lopez Ortiz P. Neovagina in vaginal agenesis: surgical methods and long term results. J Pediatr Surg 27:10–14
McCraw JB, Massery FM, Shanklin KD, Horton CE (1976) Vaginal reconstruction with Gracilis myocutaneous flaps. Plastic Reconstruct. Surg 52:176–183
Huang TT (1995) Twenty years of experience in managing gender dysphoria patients: I. Surgical management of male transsexuals. Plastic Reconstruct. Surg 96:921–930
Chudacoff RM, Alexander J, Alvero R, Segars JH (1996) Tissue expansion vaginoplasty for treatment of congenial vaginal agenesis. Obstet Gynecology 87:865–868
Flack C, Barbara MA, Steven PS (1993) Vaginoplasty: combination therapy using labia minora flaps and Lucite dilators: a preliminary report. J Urol 150:654–656
Morton KE, Davies D, Demurest C (1986) The use of fasciocutaneous flap in vaginal reconstruction. Brit J Obstet Gynecol 93:970–973
Joseph VT (1997) Pudendal thigh-flap vaginoplasty in reconstruction of genital anomalies. J Pediatric Surg 32:62–65
Selvaggi G, Monstrey S, Depypere H, Blondeel P, Van Landuyt K, Hamdi M, Dhont M (2003) Creation of neovagina with use of a pudendal thigh fasciocutaneous flap and restoration of uterovaginal continuity. Fertil Steril 80:607–611
Pakiam AI (2008) Medial thigh flaps for repair of vaginal stenosis. Grabb’s encyclopedia of flaps, vol 3, Torso, Pelvis and Lower Extremities, Editors B. Strauch et al, 3rd Edition, Lippicott and Williams; Baltimore, 2008, pp 1168-1169
Panici PB, Bellati F, Boni T, Francescangeli F, Frati L, Marchese C (2007) Vaginoplasty using autologous in vitro cultured vaginal tissue in a patient with Mayer–von-Rokitansky–Kutser–Hauser syndrome. Human Reproduction 22:2025–2028
Barutçu A, Akgüner M (1998) McIndoe vaginoplasty with the inflatable vaginal stent. Ann Plast Surg 41(5):568–569
Reed H (2011) Aesthetic and functional male to female genital and perineal surgery: feminizing vaginoplasty. Semi Plast Surg 25:163–174
Siemssen PA, Matzen SH (1997) Neovaginal construction in vaginal aplasia and sexual reassignment surgery. Scand J Plast Reconstr Hand Surg 31:47–50
Stein M, Defer C, Merman A (1990) Followup observations of male to female transsexuals. J Urol 143:1188–1192
Sheares BH (1960) Congenital atresia of the vagina: a new technique for tunneling the space between bladder and rectum and construction of the new vagina by a modified Wharton technique. J Obstet Gynaecol Br Emp 67:24–31
Pulman KJ, Kives S, Jamieson MA (2012) A case of vaginoplasty without grafting. J Pediatr Adolesc Gynecol 25:e17–e19
Jayaram BN, Stuteville OH, Bush IM (1978) Complications and undesirable results of sex-reassignment surgery in male-to-female transsexuals. Arch Sex Behav 7:337–345
Coskun A, Coban YK, Vardar MA, Dalay AC (2007) BioMed Central Surg 7:1–4
Boston University School of Medicine, Department of Sexual Medicine (internet posting) http://www.bumc.bu.edu/sexualmedicine/physicianinformation/female-genital-anatomy/sexualfunction. Urol Clin N Am 2002; 29:685–693
Dietrich W, Haitel A, Huber JC, Reiter WJ (2004) Expression of estrogen receptors in human corpus cavernosum and male urethra. J Histochem and Cytochem 52:355
Thornton JM (2013) Estrogens and aging skin. Dermato-Endocrinology 5:264–270
Son ED, Lee JY, Lee S, Kim MS, Lee BG, Chang IS et al (2005) Topical application of 17 beta-estradiol increases extra cellular matrix protein synthesis by stimulating tgf-beta signaling in aged human skin in vivo. J Invest Dermatol 124:1149–1161
Thornton MJ (2005) Oestrogen functions in skin and skin appendages. Expert Opin 9:617–629
Acknowledgments
The authors wish to thank Ethel R Slater, associate librarian at the Mount Sinai Medical Center Medical Library for her tireless efforts and George Wayne, statistician for his analysis and commentary.
Conflict of interest
The authors declare they have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reed, H.M., Yanes, R.E., Delto, J.C. et al. Non-grafted Vaginal Depth Augmentation for Transgender Atresia, Our Experience and Survey of Related Procedures. Aesth Plast Surg 39, 733–744 (2015). https://doi.org/10.1007/s00266-015-0523-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-015-0523-7