Abstract
Background
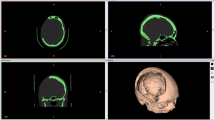
Cranioplasty using alternate alloplastic bone substitutes instead of autologous bone grafting is inevitable in the clinical field. The authors present their experiences with cranial reshaping using methyl methacrylate (MMA) and describe technical tips that are keys to a successful procedure.
Methods
A retrospective chart review of patients who underwent cranioplasty with MMA between April 2007 and July 2010 was performed. For 20 patients, MMA was used for cranioplasty after craniofacial trauma (n = 16), tumor resection (n = 2), and a vascular procedure (n = 2). The patients were divided into two groups. In group 1, MMA was used in full-thickness inlay fashion (n = 3), and in group 2, MMA was applied in partial-thickness onlay fashion (n = 17). The locations of reconstruction included the frontotemporal region (n = 5), the frontoparietotemporal region (n = 5), the frontal region (n = 9), and the vertex region (n = 1). The size of cranioplasty varied from 30 to 144 cm2.
Results
The amount of MMA used ranged from 20 to 70 g. This biomaterial was applied without difficulty, and no intraoperative complications were linked to the applied material. The patients were followed for 6 months to 4 years (mean, 2 years) after MMA implantation. None of the patients showed any evidence of implant infection, exposure, or extrusion. Moreover, the construct appeared to be structurally stable over time in all the patients.
Conclusions
Methyl methacrylate is a useful adjunct for treating deficiencies of the cranial skeleton. It provides rapid and reliable correction of bony defects and contour deformities. Although MMA is alloplastic, appropriate surgical procedures can avoid problems such as infection and extrusion. An acceptable overlying soft tissue envelope should be maintained together with minimal contamination of the operative site.
Level of Evidence V
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.






Similar content being viewed by others
References
Miyake H, Ohta T, Tanaka H (2000) A new technique for cranioplasty with L-shaped titanium plates and combination ceramic implants composed of hydroxyapatite and tricalcium phosphate (Ceratite). Neurosurgery 46:414–418
Gasparini G, Boniello R, Moro A, Tamburrini G, Di Rocco C, Pelo S (2009) Cranial reshaping using methyl methacrylate: technical note. J Craniofac Surg 20:184–190
Marchac D, Greensmith A (2008) Long-term experience with methyl methacrylate cranioplasty in craniofacial surgery. J Plast Reconstr Aesthet Surg 61:744–752 discussion 753
Li CH, Yang SH, Wang HS, Tu YK, Kuo MF (2010) Use of the “mortise and tenon” principle in the augmentation of autologous cranioplasty using bone cement in a child. Childs Nerv Syst 26:1807–1811
Sahoo N, Roy ID, Desai AP, Gupta V (2010) Comparative evaluation of autogenous calvarial bone graft and alloplastic materials for secondary reconstruction of cranial defects. J Craniofac Surg 21:79–82
Badie B (1996) Cosmetic reconstruction of temporal defect following pterional [corrected] craniotomy. Surg Neurol 45:383–384
Afifi A, Djohan RS, Hammert W, Papay FA, Barnett AE, Zins JE (2010) Lessons learned reconstructing complex scalp defects using free flaps and a cranioplasty in one stage. J Craniofac Surg 21:1205–1209
Ducic Y (2002) Titanium mesh and hydroxyapatite cement cranioplasty: a report of 20 cases. J Oral Maxillofac Surg 60:272–276
Hammon WM, Kempe LG (1971) Methyl methacrylate cranioplasty: 13 years experience with 417 patients. Acta Neurochir Wien 25:69–77
Belmahi A, Gharib NE, Bencheikh R, Abbassi A, Mizahi M (2002) Reconstruction of large scalp and calvarium defects by using the semi-free latissimus dorsi flap associated with methyl methacrylate implant for cranioplasty. Ann Chir Plast Esthet 47:298–303
Yanai A (1991) Resin sealant: a new method of methyl methacrylate cranioplasty (technical note). J Neurosurg 75:328–330
Elshahat A, Shermak MA, Inoue N, Chao EY, Manson P (2004) The use of Novabone and Norian in cranioplasty: a comparative study. J Craniofac Surg 15:483–489
Jackson IJ, Hoffmann GT (1956) Depressed comminuted fracture of a plastic cranioplasty. J Neurosurg 13:116–117
Matic DB, Manson PN (2004) Biomechanical analysis of hydroxyapatite cement cranioplasty. J Craniofac Surg 15:415–422 discussion 422–423
Benzel EC, Thammavaram K, Kesterson L (1990) The diagnosis of infections associated with acrylic cranioplasties. Neuroradiology 32:151–153
Shapiro SA (1991) Cranioplasty, vertebral body replacement, and spinal fusion with tobramycin-impregnated methyl methacrylate. Neurosurgery 28:789–791
Manson PN, Crawley WA, Hoopes JE (1986) Frontal cranioplasty: risk factors and choice of cranial vault reconstructive material. Plast Reconstr Surg 77:888–904
Matsuno A, Tanaka H, Iwamuro H, Takanashi S, Miyawaki S, Nakashima M, Nakaguchi H, Nagashima T (2006) Analyses of the factors influencing bone graft infection after delayed cranioplasty. Acta Neurochir Wien 148:535–540 discussion 540
Cheng YK, Weng HH, Yang JT, Lee MH, Wang TC, Chang CN (2008) Factors affecting graft infection after cranioplasty. J Clin Neurosci 15:1115–1119
Magee WP Jr, Ajkay N, Freda N, Rosenblum RS (2004) Use of fast-setting hydroxyapatite cement for secondary craniofacial contouring. Plast Reconstr Surg 114:289–297
Cabraja M, Klein M, Lehmann TN (2009) Long-term results following titanium cranioplasty of large skull defects. Neurosurg Focus 26:E10
Davies JP, Harris WH (1995) Comparison of diametral shrinkage of centrifuged and uncentrifuged Simplex P bone cement. J Appl Biomater 6:209–211
Fernandez E, Ginebra MP, Boltong MG, Driessens FC, Ginebra J, De Maeyer EA, Verbeeck RM, Planell JA (1996) Kinetic study of the setting reaction of a calcium phosphate bone cement. J Biomed Mater Res 32:367–374
Fujishiro Y, Takahashi K, Sato T (2001) Preparation and compressive strength of alpha-tricalcium phosphate/gelatin gel composite cement. J Biomed Mater Res 54:525–530
Costantino PD, Friedman CD, Lane A (1993) Synthetic biomaterials in facial plastic and reconstructive surgery. Facial Plast Surg 9:1–15
Verheggen R, Merten HA (2001) Correction of skull defects using hydroxyapatite cement (HAC)—evidence derived from animal experiments and clinical experience. Acta Neurochir Wien 143:919–926
Moreira-Gonzalez A, Jackson IT, Miyawaki T, Barakat K, DiNick V (2003) Clinical outcome in cranioplasty: critical review in long-term follow-up. J Craniofac Surg 14:144–153
Tadros M, Costantino PD (2008) Advances in cranioplasty: a simplified algorithm to guide cranial reconstruction of acquired defects. Facial Plast Surg 24:135–145
Robinson AC, O’Dwyer TP, Gullane PJ, Dolan EJ (1989) Anterior skull defect reconstruction with methyl methacrylate. J Otolaryngol 18:241–244
Acknowledgment
The authors have no financial interest to declare in relation to the content of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Han, SE., Lim, S.Y., Pyon, JK. et al. Aesthetic Refinement of Secondary Cranioplasty Using Methyl Methacrylate Bone Cements. Aesth Plast Surg 37, 592–600 (2013). https://doi.org/10.1007/s00266-013-0110-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-013-0110-8