Abstract
Background
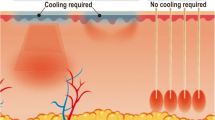
Several surgical strategies have evolved for the treatment of focal axillary hyperhidrosis (FAH). However, nonresponders are found in every procedure. Until now no characterization of the recurrent sweating areas has been reported. The aim of this study was to characterize the axillary sweat area by using the iodine starch test in nonresponders prior to surgery.
Methods
Prior to minimally invasive surgery, 24 (15 females, 9 males) nonresponders underwent a repetitive iodine starch test to define the area of recurrent sweating. Size and distribution of the hyperhidrotic area were documented.
Results
Eighteen patients had undergone previous liposuction and six liposuction curettage. The size of recurrent sweating area was 10.2 cm2 (range = 5.5–24.5 cm2). We were able to identify three different patterns of recurrent sweating: crescent (33%), circular (41%), and insertion-spot type (26%).
Conclusion
Patterns of recurrent sweating areas may partially indicate insufficient planning and implementation of surgery, resulting in nonresponders. We suggest that exact preoperative identification of the hyperhidrotic area be mandatory.

Similar content being viewed by others
References
Böni R (2006) Tumescent suction curettage in the treatment of axillary hyperhidrosis: experience in 63 patients. Dermatology 213:215–217
Lee D, Cho SH, Kim YC, Park JH, Lee SS, Park SW (2006) Tumescent liposuction with dermal curettage for treatment of axillary osmidrosis and hyperhidrosis. Dermatol Surg 32:505–511
Tung TC, Wei FC (1997) Excision of subcutaneous tissue for the treatment of axillary osmidrosis. Br J Plast Surg 50:61–66
Bechara FG, Sand M, Sand D, Altmeyer P, Hoffmann K (2007) Suction-curettage as a surgical treatment of focal axillary hyperhidrosis: recommendation for an aggressive approach. Plast Reconstr Surg 119:1390–1391
Definition and therapy of primary hyperhidrosis. Guidelines of the German Society of Dermatology (DDG), February 2007. Available at http://www.uni-duesseldorf.de/AWMF/ll/013-059.htm. Accessed 27 Oct 2008
Bechara FG, Gambichler T, Bader A, Sand M, Altmeyer P, Hoffmann K (2007) Assessment of quality of life in patients with primary axillary hyperhidrosis before and after suction-curettage. J Am Acad Dermatol 57:207–212
Bechara FG, Sand M, Sand D, Altmeyer P, Hoffmann K (2006) Surgical treatment of axillary hyperhidrosis: a study comparing liposuction cannulas with a suction-curettage cannula. Ann Plast Surg 56:654–657
Park YJ, Shin MS (2001) What is the best method for treating osmidrosis? Ann Plast Surg 47:303–309
Perng CK, Yeh FL, Ma H, Lin JT, Hwang CH, Shen BH, Chen CH, Fang RH (2004) Is the treatment of axillary osmidrosis with liposuction better than open surgery? Plast Reconstr Surg 114:93–97
Heckmann M, Rzany B (2002) Botulinumtoxin in der Dermatologie. Grundlagen und praktische Anwendung. Urban & Vogel, München
Lawrence CM, Lonsdale Eccles AA (2006) Selective sweat gland removal with minimal skin excision in the treatment of axillary hyperhidrosis: a retrospective clinical and histological review of 15 patients. Br J Dermatol 155:115–118
Minor V (1929) Ein neues Verfahren zu der klinischen Untersuchung der Schweißabsonderung. Dtsch Z Nervenheilk 101:302–308
Bechara FG, Sand M, Sand D, Achenbach RK, Altmeyer P, Hoffmann K (2006) Focal hyperhidrosis of the anal fold: a simple technique for diagnosis and evaluation of therapy. Br J Dermatol 155:858
Tsai RY, Lin JY (2001) Experience of tumescent liposuction in the treatment of osmidrosis. Dermatol Surg 27:446–448
Naumann M, Lowe NJ, Kumar CR, Hamm H (2003) Botulinum toxin type A is a safe and effective treatment for axillary hyperhidrosis over 16 months: a prospective study. Arch Dermatol 139:731–736
Bechara FG, Sand M, Hoffmann K, Boorboor P, Altmeyer P, Stucker M (2008) Histological and clinical findings in different surgical strategies for focal axillary hyperhidrosis. Dermatol Surg 34:1001–1009
Author information
Authors and Affiliations
Corresponding author
Additional information
F. G. Bechara and M. Sand have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Bechara, F.G., Sand, M. & Altmeyer, P. Characteristics of Refractory Sweating Areas Following Minimally Invasive Surgery for Axillary Hyperhidrosis. Aesth Plast Surg 33, 308–311 (2009). https://doi.org/10.1007/s00266-008-9261-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-008-9261-4