Abstract
Aim of the study
To compare the efficacy of spinal anaesthesia alone versus spinal anesthesia augmented with ultrasound-guided pericapsular nerve group (PENG) block combined with lateral femoral cutaneous nerve (LFCN) block in improving perioperative analgesia and functional recovery in patients undergoing THA.
Methods
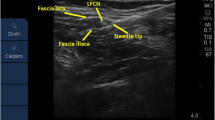
In a prospective, randomized clinical trial we included 66 patients scheduled for THA were divided into two groups: one receiving spinal anaesthesia alone (SA group; n = 32) and the other receiving spinal anaesthesia with regional analgesia blocks PENG + LFCN (SRAB group; n = 34). In the SRAB group, PENG followed by LFCN blocks were administered under ultrasound guidance before spinal anaesthesia.
Results
There were significant differences between the two groups in the onset of postoperative pain (p < 0.01) and the total amount of analgesics required in the first 36 postoperative hours (p < 0.01).
Conclusion
The combined approach of spinal anaesthesia with PENG and LFCN blockade, enables opioid-free analgesia and may contribute to a safer and more comfortable postoperative experience for THA patients.







Similar content being viewed by others
Data availability
All research related materials and data are stored at the Orthopedic Department of the General Hospital Gradiska, Mladen Stojanovic street No 10, Gradiska, Bosnia and Herzegovina.
References
GBD (2019) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study. https://vizhub.healthdata.org/gbd-results/. Accesed 20 February 2024
Pabinger C, Lothaller H, Portner N, Geissler A (2018) Projections of hip arthroplasty in OECD countries up to 2050. Hip Int 28(5):498–506. https://doi.org/10.1177/1120700018757940
Sharrock NE, Cazan MG, Hargett MJ, Williams-Russo P, Wilson PD Jr (1995) Changes in mortality after total hip and knee arthroplasty over a ten-year period. Anesth Analg 80(2):242–248. https://doi.org/10.1097/00000539-199502000-00008
Girón-Arango L, Peng PWH, Chin KJ, Brull R, Perlas A (2018) Pericapsular Nerve Group (PENG) Block for Hip Fracture. Reg Anesth Pain Med 43(8):859–863. https://doi.org/10.1097/AAP.0000000000000847
Roy R, Agarwal G, Pradhan C, Kuanar D (2019) Total postoperative analgesia for hip surgeries, PENG block with LFCN block. Regional anesthesia and pain medicine rapm-2019–100454. https://doi.org/10.1136/rapm-2019-100454
Girón-Arango L, Roqués V, Peng P (2019) Reply To Dr Roy et al: Total postoperative analgesia for hip surgeries: PENG block with LFCN block. Regional anesthesia and pain medicine rapm-2019–100505. https://doi.org/10.1136/rapm-2019-100505
Chua H, Brady B, Farrugia M, Pavlovic N, Ogul S, Hackett D, Farag D, Wan A, Adie S, Gray L, Nazar M, Xuan W, Walker RM, Harris IA, Naylor JM (2020) Implementing early mobilisation after knee or hip arthroplasty to reduce length of stay: a quality improvement study with embedded qualitative component. BMC Musculoskelet Disord 21(1):765. https://doi.org/10.1186/s12891-020-03780-7
Gan TJ (2017) Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res 10:2287–2298. https://doi.org/10.2147/JPR.S144066
Morrison SR, Magaziner J, McLaughlin MA, Orosz G, Silberzweig SB, Koval KJ, Siu AL (2003) The impact of post-operative pain on outcomes following hip fracture. Pain 103(3):303–311. https://doi.org/10.1016/S0304-3959(02)00458-X
Duggleby W, Lander J (1994) Cognitive status and postoperative pain: older adults. J Pain Symptom Manage 9(1):19–27. https://doi.org/10.1016/0885-3924(94)90142-2
Kolomachenko V (2021) Eficiency of Pericapsulare nerve group block after hip arthroplasty. Georgian Med News 320:18–22
Patel V, Patel V, Abdallah F, Whelan D, Bansal S, Gabra M, Brull R (2022) The analgesic benefit of Pericapsular Nerve Group (PENG) block in hip arthroscopic surgery: a retrospective pragmatic analysis at an academic health center. Regional anesthesia and pain medicine rapm-2022–103743. https://doi.org/10.1136/rapm-2022-103743
Mauermann WJ, Shilling AM, Zuo Z (2006) A comparison of neuraxial block versus general anesthesia for elective total hip replacement: a meta-analysis. Anesth Analg 103(4):1018–1025. https://doi.org/10.1213/01.ane.0000237267.75543.59
Modig J (1988) Regional anaesthesia and blood loss. Acta Anaesthesiol Scand Suppl 89:44–48. https://doi.org/10.1111/j.1399-6576.1988.tb02842.x
Palija S, Bijeljac S, Manojlovic S, Jovicic Z, Jovanovic M, Cvijic P, Dragicevic-Cvjetkovic D (2021) Effectiveness of different doses and routes of administration of tranexamic acid for total hip replacement. Int Orthop 45(4):865–870. https://doi.org/10.1007/s00264-020-04585-y
Funding
There was no additional costs during implementation of observational study. All costs caused by examinations and analyses are routinely performed to patients who undergo total hip replacement. No financial resources or fees were given to the authors. The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
The study conception and design were contributed by Anita Djurdjevic Svraka and Slavko Manojlovic. Material preparation, data collection, and analysis were performed by Anita Djurdjevic Svraka, Dragan Svraka, Aleksandar Milivojac, Rajko Dodik, Slavko Manojlovic, Stanislav Palija. The first draft of the manuscript was written by Anita Djurdjevic Svraka, and all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Approval was obtained from the Ethics Committee of General Hospital Gradiska. The Ethics Committee worked exclusively in accordance with the ICH-GCP rules and the latest version of the Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data and photographs.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Svraka, A.D., Svraka, D., Milivojac, A. et al. Enhancing postoperative recovery in total hip arthroplasty: the role of pericapsular nerve group and lateral cutaneous nerve block under spinal anaesthesia. International Orthopaedics (SICOT) (2024). https://doi.org/10.1007/s00264-024-06187-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00264-024-06187-4