Abstract
Purpose
Selecting a postgraduate medical or surgical specialty is a significant decision for medical students, influenced by factors such as demographics, academic performance, satisfaction, work environments, personal aspirations, passion for a specific specialty, exposure to different fields during medical education, lifestyle considerations, financial factors, job market conditions, and prospects. Our research focused on orthopaedic surgery, a highly competitive specialty with many applicants and a low acceptance rate. We aimed to investigate the factors that contribute to the sustained interest in this specialty despite the challenges of securing a residency position. Hence, this study aims to examine the potential factors that influence students' decision to pursue a career as an orthopaedic surgeon.
Methods
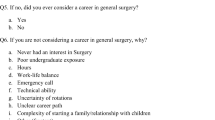
This cross-sectional study explores the perspectives and attitudes of 211 fifth-year medical students towards orthopaedic surgery after completing their clinical rotation at Mutah University's School of Medicine in 2022. The inclusion criteria for the study were limited to fifth-year medical students who successfully finished the orthopaedic rotation. A questionnaire was employed to evaluate students' firm commitment to orthopaedics as a prospective career and the degree of their current interest in the specialty.
Results
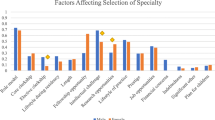
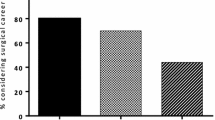
The study involved 210 participants, with 99 selecting orthopaedics as their specialty and 111 pursuing alternatives. Furthermore, 41.4% expressed the intention to apply for orthopaedic residencies. Factors impacting orthopaedics selection included family/peer input (p = 0.002), prestige (p = 0.002), research prospects (p = 0.005), leadership potential (p = 0.011). Chi-square analysis showed associations between choosing orthopaedics and male gender (p = 0.028), parental occupation in musculoskeletal fields (p = 0.038), and elective rotations (p = 0.016).
Conclusion
This study examines the factors that influence medical students’ career preferences in orthopaedic surgery, highlighting the significance of familial and peer influences, job prestige perceptions, gender considerations, parental involvement, elective rotations, research and teaching potential assessments, and aspirations for leadership roles. These findings reveal the complex array of factors that guide medical students toward orthopaedic surgery.

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available but may be made available by the corresponding author on reasonable request.
Code availability
Not applicable.
References
Kalén S, Stenfors-Hayes T, Hylin U, Larm MF, Hindbeck H, Ponzer S (2010) Mentoring medical students during clinical courses: a way to enhance professional development. Med Teach 32(8). https://doi.org/10.3109/01421591003695295
Derck J et al (2018) Exploring the impact factor: medical students mentoring high school students and cultivating cultural humility. Health Equity 2(1):15. https://doi.org/10.1089/HEQ.2017.0025
Allen S, Olson A, Menk J, Nixon J (2017) Hypothesis-driven physical examination curriculum. Clin Teach 14(6):417–422. https://doi.org/10.1111/TCT.12581
Stansfield RB et al (2016) Assessing musculoskeletal examination skills and diagnostic reasoning of 4th-year medical students using a novel objective structured clinical exam. BMC Med Educ 16(1):1–7. https://doi.org/10.1186/S12909-016-0780-4/TABLES/3
Shrivastava S, Shrivastava P (2021) Training medical students to develop the skills for establishing clinical diagnosis. J Sci Soc 48(1):10. https://doi.org/10.4103/JSS.JSS_123_20
Cebeci S, Dane S, Kaya M, Yigitoglu R (2013) Medical students’ approaches to learning and study skills. Procedia Soc Behav Sci 93:732–736. https://doi.org/10.1016/J.SBSPRO.2013.09.271
Joshi A, Ganjiwale J, Varma J, Singh P, Modi J, Singh T (2017) Qualitative assessment of learning strategies among medical students using focus group discussions and in-depth interviews. Int J Appl Basic Med Res 7(5):33. https://doi.org/10.4103/IJABMR.IJABMR_144_17
Kusurkar R, Kusurkar R (2012) Motivation in medical students: a PhD thesis report. Perspect Med Educ 1(3):155–157. https://doi.org/10.1007/S40037-012-0016-1
McConnell MM, Eva KW (2012) The role of emotion in the learning and transfer of clinical skills and knowledge. Acad Med 87(10):1316–1322. https://doi.org/10.1097/ACM.0B013E3182675AF2
Morokhovets HY, Lysanets YV (2017) Developing the professional competence of future doctors in the instructional setting of higher medical educational institutions. Wiadomości Lekarskie 70(1):101–104
Pelaccia T, Viau R (2017) Motivation in medical education. Med Teach 39(2):136–140. https://doi.org/10.1080/0142159X.2016.1248924
Ten Cate TJ, Kusurkar RA, Williams GC (2011) How self-determination theory can assist our understanding of the teaching and learning processes in medical education. AMEE guide No. 59. Med Teach 33(12):961–973. https://doi.org/10.3109/0142159X.2011.595435
Artino AR, La Rochelle JS, Durning SJ (2010) Second-year medical students’ motivational beliefs, emotions, and achievement. Med Educ 44(12):1203–1212. https://doi.org/10.1111/J.1365-2923.2010.03712.X
Contributions M, Sud S, Wong JP, Premji L, Punnett A (2020) Career decision making in undergraduate medical education / Décisions à prendre quant au choix de carrière au cours des études de premier cycle en médecine. Can Med Educ J 2020(3):56–66. https://doi.org/10.36834/cmej.69220
Moore BA, Barnett JE (2019) Making decisions. Case studies in clinical psychological science: bridging the gap from science to practice, 1–7. https://doi.org/10.1093/MED/9780199681907.003.0053
Marshall AL, Thompson CA, Cullen MW, Raffals LE, Oxentenko AS (2020) Medical education interest, exposure, and career planning in subspecialty trainees. Med Sci Educ 30(3):1011. https://doi.org/10.1007/S40670-020-01007-X
Thornton J (2000) Physician choice of medical specialty: do economic incentives matter? Appl Econ 32(11):1419–1428. https://doi.org/10.1080/00036840050151494
Thornton J, Esposto F (2003) How important are economic factors in the choice of medical specialty? Health Econ 12(1):67–73. https://doi.org/10.1002/HEC.682
Kim H et al (2003) Factors influencing the specialty selection of medical students. Korean J Med Educ 15(2):151–161. https://doi.org/10.3946/KJME.2003.15.2.151
Hohf-Nova M, Hun-Pacheco R, Munoz-Bustos D, Soto-Carriel A, Perez-Villalobos C (2021) When it is time to decide: factors associated with the choice of a medical specialty. Rev Med Chil 149(9):1352–1359. https://doi.org/10.4067/S0034-98872021000901352
Johnson AL et al (2012) Why do medical students choose orthopaedics as a career? J Bone Joint Surg Am 94(11). https://doi.org/10.2106/JBJS.K.00826
DePasse JM, Palumbo MA, Eberson CP, Daniels AH (2016) Academic characteristics of orthopaedic surgery residency applicants from 2007 to 2014. J Bone Joint Surg Am 98(9):788–795. https://doi.org/10.2106/JBJS.15.00222
Rynecki N et al (2020) An analysis of trends in national residency matching program match data for orthopedic surgery. Orthopedics 43(6). https://doi.org/10.3928/01477447-20200910-03
Mowbray RM, Davies B (1971) Personality factors in choice of medical specialty. Br J Med Educ 5(2):110–117. https://doi.org/10.1111/J.1365-2923.1971.TB02013.X
Johnson JW, Graham L, Williams E, Campbell C, Thomas N, Gossell-Williams M (2022) Clinical elective choices and motivations for future career specialty selection of medical school trainees and junior doctors of the University of the West Indies, Jamaica. Int J Med Stud 10(1):49–55. https://doi.org/10.5195/IJMS.2021.1049
Weissman C et al (2012) Medical specialty considerations by medical students early in their clinical experience. Israel J Health Policy Res 1(1):1–10. https://doi.org/10.1186/2045-4015-1-13/COMMENTS
Chen H, Hardacre JM, Martin C, Lillemoe KD (2001) Do medical school surgical rotations influence subspecialty choice? J Surg Res 97(2):172–178. https://doi.org/10.1006/JSRE.2001.6135
Olsson C, Kalén S, Ponzer S (2019) Sociological analysis of the medical field: using Bourdieu to understand the processes preceding medical doctors’ specialty choice and the influence of perceived status and other forms of symbolic capital on their choices. Adv Health Sci Educ 24(3):443–457. https://doi.org/10.1007/S10459-018-09872-3/FIGURES/1
Creed PA, Searle J, Rogers ME (2010) Medical specialty prestige and lifestyle preferences for medical students. Soc Sci Med 71(6):1084–1088. https://doi.org/10.1016/J.SOCSCIMED.2010.06.027
Norredam M, Album D (2007) Prestige and its significance for medical specialties and diseases. Scand J Public Health 35(6):655–661. https://doi.org/10.1080/14034940701362137
Yazigi A, Nassr M, Sleilaty G, Nemr E (2006) The influence of clinical teachers as role models on the choice of specialty among Lebanese medical students. J Med Liban 54(1):37
Maiorova T, Stevens F, Scherpbier A, Van Der Zee J (2008) The impact of clerkships on students’ specialty preferences: what do undergraduates learn for their profession? Med Educ 42(6):554–562. https://doi.org/10.1111/J.1365-2923.2008.03008.X
Fincher RME, Lewis LA (1993) Specialty choice: development of a questionnaire. Med Educ 27(5):446–451. https://doi.org/10.1111/J.1365-2923.1993.TB00299.X
Jarecky RK, Schwartz RW, Haley JV, Donnelly MB (1991) Stability of medical specialty selection at the University of Kentucky. Acad Med 66(12):756–761. https://doi.org/10.1097/00001888-199112000-00011
Guraya SY, Almaramhy HH (2018) Mapping the factors that influence the career specialty preferences by the undergraduate medical students. Saudi J Biol Sci 25(6):1096–1101. https://doi.org/10.1016/J.SJBS.2017.03.019
Hoeffel D et al (2023) Systematic review and meta-analysis of economic and healthcare resource utilization outcomes for robotic versus manual total knee arthroplasty. J Robot Surg 17(6):2899–2910. https://doi.org/10.1007/S11701-023-01703-X/FIGURES/4
Massey PA et al (2023) Improved outcomes after reinforced radial Meniscus repair augmented with bone marrow aspirate concentrate. Arthrosc Sports Med Rehabil 5(3):e843. https://doi.org/10.1016/J.ASMR.2023.04.014
Bansal S et al (2021) Meniscal repair: the current state and recent advances in augmentation. J Orthop Res 39(7):1368. https://doi.org/10.1002/JOR.25021
Ellinger F, Tropp H, Gerdhem P, Hallgren HB, Ivars K (2023) Magnetically controlled growing rod treatment for early-onset scoliosis: analysis of 52 consecutive cases demonstrates improvement of coronal deformity. J Spine Surg 9(3):259–268. https://doi.org/10.21037/JSS-22-70
Xu L et al (2021) Clinical study of 3D printed personalized prosthesis in the treatment of bone defect after pelvic tumor resection. J Orthop Transl 29:163. https://doi.org/10.1016/J.JOT.2021.05.007
Acknowledgements
The authors appreciate the technical support of all the radiology staff.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study's conception and design. Material preparation, data collection, and analysis were performed by Mohammad N. Alswerki. The first draft of the manuscript was written by Moh'd S. Dawod and all authors commented on previous versions of the manuscript. The analysis was done by Mothana Al-Takhaineh. The discussion section, the conclusion, and the abstract were done by Mohammad Alswerki. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Mutah University (IRB approval number 123/2023).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
The authors affirm that human research participants provided informed consent for publication of the results of this research.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of evidence: Level IV, cross-sectional study
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dawod, M.S., Alswerki, M.N. & Al-Takhaineh, M.A. Factors that influence medical students’ decision to pursue a career in orthopaedics: a comprehensive analysis. International Orthopaedics (SICOT) 48, 1139–1147 (2024). https://doi.org/10.1007/s00264-024-06132-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-024-06132-5