Abstract
Purpose
The optimal timing of surgery after traumatic rotator cuff tears (RCT) is unclear, with its impact on functional outcomes under debate. This study aimed to review functional outcomes after RCT repair in patients who underwent early vs delayed surgery at our unit.
Methods
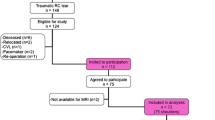
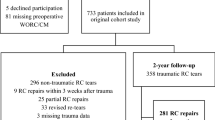
This was single-centre retrospective evaluation. Patients with an acute traumatic RCT that underwent repair between 2017 and 2019 and had local follow-up were included and placed into two groups: early surgery (within 6 months from injury) and delayed surgery (more than 6 months from injury). Patient demographics, RCT data and pre- and post-operative (after 12 months) Oxford Shoulder Score (OSS) were extracted from medical records. Data was analysed to compare OSS scores between groups, as well as the effect of cuff tear sizes on OSS scores.
Results
Forty-nine patients were included in the analysis (15 early, 34 delayed). There were no significant differences in age, sex or cuff tear sizes between groups. No difference was identified in the mean post-operative OSS between early vs delayed groups (40.9 ± 6.34 vs 40.5 ± 7.65, p = 0.86). The mean improvement in OSS after surgery was also similar between groups (22.5 ± 7.81 vs 20.97 ± 7.19, p = 0.498). Having a large or massive RCT did not worsen OSS compared to small or medium RCT (p = 0.44), even when stratified by early or delayed surgery.
Conclusion
Delayed surgery for traumatic RCT greater than 6 months from injury did not negatively impact long-term functional outcomes at our unit. Patients should be reassured as applicable before surgery in the event of prolonged or unavoidable delays.
Similar content being viewed by others
Data availability
The dataset used in this study to evaluate practice is not openly available due to reasons of sensitivity and confidentiality. Reasonable requests for access may be considered by contacting the corresponding author.
References
Bedi A, Dines J, Warren RF, Dines DM (2010) Massive tears of the rotator cuff. J Bone Joint Surg 92(9):1894–1908. https://doi.org/10.2106/jbjs.i.01531
Minns Lowe CJ, Moser J, Barker K (2014) Living with a symptomatic rotator cuff tear ‘bad days, bad nights’: a qualitative study. BMC Musculoskelet Disord 15:228. https://doi.org/10.1186/1471-2474-15-228
Zhaeentan S, Von Heijne A, Stark A, Hagert E, Salomonsson B (2015) Similar results comparing early and late surgery in open repair of traumatic rotator cuff tears. Knee Surg Sports Traumatol Arthrosc 24(12):3899–3906. https://doi.org/10.1007/s00167-015-3840-0
Björnsson HC, Norlin R, Johansson K, Adolfsson LE (2011) The influence of age, delay of repair, and tendon involvement in acute rotator cuff tears. Acta Orthop 82(2):187–192. https://doi.org/10.3109/17453674.2011.566144
Dimmen S, Owesen C, Lundgreen K, Jenssen KK (2022) No difference in clinical outcome after rotator cuff repair performed within or later than 3 months after trauma: a retrospective cohort study. Knee Surg Sports Traumatol Arthrosc 31(2):672–680. https://doi.org/10.1007/s00167-022-07193-y
Duncan NS, Booker SJ, Gooding BWT, Geoghegan J, Wallace WA, Manning PA (2015) Surgery within 6 months of an acute rotator cuff tear significantly improves outcome. J Shoulder Elbow Surg 24(12):1876–1880. https://doi.org/10.1016/j.jse.2015.05.043
Hantes ME, Karidakis GK, Vlychou M, Varitimidis S, Dailiana Z, Malizos KN (2011) A comparison of early versus delayed repair of traumatic rotator cuff tears. Knee Surg Sports Traumatol Arthrosc 19(10):1766–1770. https://doi.org/10.1007/s00167-011-1396-1
Fu MC, O’Donnell EA, Taylor SA, Aladesuru OM, Rauck RC, Dines JS, Dines DM, Warren RF, Gulotta LV (2020) Delay to arthroscopic rotator cuff repair is associated with increased risk of revision rotator cuff surgery. Orthopedics 43(6):340–344. https://doi.org/10.3928/01477447-20200923-02
Gutman MJ, Joyce CD, Patel MS, Kirsch JM, Gutman BS, Abboud JA, Namdari S, Ramsey ML (2021) Early repair of traumatic rotator cuff tears improves functional outcomes. J Shoulder Elbow Surg 30(11):2475–2483. https://doi.org/10.1016/j.jse.2021.03.134
Mukovozov I, Byun S, Farrokhyar F, Wong I (2013) Time to surgery in acute rotator cuff tear. Bone Joint Res 2(7):122–128. https://doi.org/10.1302/2046-3758.27.2000164
Leow JM, Krahelski O, Keenan OJ, Clement ND, McBirnie JM (2020) Functional outcome following arthroscopic repair of massive rotator cuff tears is equal to smaller rotator cuff tears: a retrospective case–control study. Shoulder Elbow 14(1 suppl):52–58. https://doi.org/10.1177/1758573220925040
Lawson O, Nicholson JA, Clement ND, Rudge W, MacDonald DJ, McBirnie J (2022) Tear size, general health status and smoking influence functional outcome at 5 years following arthroscopic rotator cuff repair. Should Elb 14(6):625–634. https://doi.org/10.1177/17585732211041637
Haviv B, Rutenberg TF, Yaari L, Khatib M, Rath E, Yassin M (2019) Which patients are less likely to improve after arthroscopic rotator cuff repair? Acta Orthop Traumatol Turc 53(5):356–359. https://doi.org/10.1016/j.aott.2019.02.003
NHS England (2023) NHS referral to treatment (RTT) waiting times data. [online] england.nhs.uk. Available at: https://www.england.nhs.uk/statistics/statistical-work-areas/rtt-waiting-times/ [Accessed 28 Oct. 2023]
British Orthopaedic Association (2022) T&O waiting list the largest for over a decade. [online] www.boa.ac.uk. Available at: https://www.boa.ac.uk/resources/t-o-waiting-list-the-largest-for-over-a-decade.html. [Accessed 06 January 2024]
Dawson J, Fitzpatrick R, Carr A (1996) Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg Br 78(4):593–600. https://doi.org/10.1302/0301-620X.78B4.0780593
Cofield RH (1982) Subscapular muscle transposition for repair of chronic rotator cuff tears. Surg Gynecol Obstet 154(5):667–672
Patel V, Thomas C, Fort H, Wood R, Modi A, Pandey R, Singh H, Armstrong A (2021) Early versus delayed repair of traumatic rotator cuff tears. Does timing matter on outcomes? Eur J Orthop Surg Traumatol 32(2):269–277. https://doi.org/10.1007/s00590-021-02962-w
Petersen SA, Murphy TP (2011) The timing of rotator cuff repair for the restoration of function. J Shoulder Elbow Surg 20(1):62–68. https://doi.org/10.1016/j.jse.2010.04.045
Weekes DG, Campbell RE, Allegretto JR, Lopez SG, Pepe MD, Tucker BS, Freedman KB, Tjoumakaris FP (2020) A prospective study of patient factors and decision-making for surgical repair of symptomatic full-thickness rotator cuff tears. Orthopedics 43(2):85–90. https://doi.org/10.3928/01477447-20191223-02
McNair AGK, MacKichan F, Donovan JL, Brookes ST, Avery KNL, Griffin SM, Crosby T, Blazeby JM (2016) What surgeons tell patients and what patients want to know before major cancer surgery: a qualitative study. BMC Cancer 16:258. https://doi.org/10.1186/s12885-016-2292-3
Tashjian RZ, Bradley MP, Tocci S, Rey J, Henn RF, Green A (2007) Factors influencing patient satisfaction after rotator cuff repair. J Shoulder Elbow Surg 16(6):752–758. https://doi.org/10.1016/j.jse.2007.02.136
Manaka T, Ito Y, Matsumoto I, Takaoka K, Nakamura H (2011) Functional recovery period after arthroscopic rotator cuff repair: is it predictable before surgery? Clin Orthop Relat Res 469(6):1660–1666. https://doi.org/10.1007/s11999-010-1689-6
Charousset C, Grimberg J, Duranthon LD, Bellaïche L, Petrover D, Kalra K (2008) The time for functional recovery after arthroscopic rotator cuff repair: correlation with tendon healing controlled by computed tomography arthrography. Arthroscopy 24(1):25–33. https://doi.org/10.1016/j.arthro.2007.07.023
van der List JP, Kok LM, Alta TDW, van der List MPJ, van Noort A (2022) Role of delay between injury and surgery on the outcomes of rotator cuff repair: a systematic review and meta-analysis. Am J Sports Med 51(5):1328–1339. https://doi.org/10.1177/03635465211069560
Abtahi AM (2015) Factors affecting healing after arthroscopic rotator cuff repair. World J Orthop 6(2):211. https://doi.org/10.5312/wjo.v6.i2.211
Funding
This work received no specific grant from any funding agency in the public, commercial, or not-for profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by RDS, AH, ES and MA-Y. The first draft of the manuscript was written by RDS, and all authors commented on previous versions of the manuscript. All authors read and approved final versions of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was registered with the local audit department of our Trust as part of an evaluation of our orthopaedic service. It followed local protocols for data collection, analysis and presentation, and ethical committee review was not required for this work as per local policy.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Sa, R., Hassan, A., Soliman, E. et al. Traumatic rotator cuff injury: does delayed surgery worsen functional outcomes?. International Orthopaedics (SICOT) 48, 1271–1275 (2024). https://doi.org/10.1007/s00264-024-06127-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-024-06127-2