Abstract
Purpose
The posterior cruciate ligament (PCL) rupture rarely occurs, especially in skeletally immature adolescents, and poses a dilemma in appropriately managing the open physis with its vast growth potential. However, although many epiphyseal-protecting techniques for anterior cruciate ligament (ACL) reconstruction have been reported, a similar problem in PCL reconstruction has received scant attention and needs more relevant research. So, this study aims to evaluate the short-term clinical and imaging results of the arthroscopic physeal-sparing reconstruction program.
Method
All the 13 patients we reviewed in this study have accepted the arthroscopic physeal-sparing PCL reconstruction from January 2019 to December 2022 in our Department of Orthopedics. Primary demographic data collected include gender (8 males and 5 females), age (11–15 years, average 13.3 years), follow-up period (15–35 months, average 25.2 months), injury mechanism (nine non-contact injuries and four contact injuries), and days following injury (1–10 days, average 5.3 days). The assessment of clinical outcomes included pre- and postoperative physical examination, knee functional scores, and imaging data.
Result
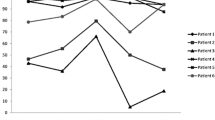
All patients in this study were followed up with an average 25.2-month (range 15–35 months) follow-up period. All the cases preoperatively had a positive posterior drawer test and turned negative at the final follow-up. The average ROM improved from 103.6° ± 11.4° to 132.6° ± 3.6° at the last follow-up (p < 0.05). The VAS score decreased from 5.8 ± 1.6 to 0.9 ± 0.5 (p < 0.05); the average KT-1000 healthy-side to affected-side difference decreased from 11.3 ± 1.6 to1.8 ± 0.5 mm. The comparison of all the knee functional scores (IKDC, Tegner scores, and Lysholm) at preoperative and last follow-up showed a significant difference (p < 0.05). None of the cases had operation-related complications, and all recovered to sports well.
Conclusion
The arthroscopic physeal-sparing posterior cruciate ligament reconstruction is a dependable and recommended treatment for posterior cruciate ligament rupture in adolescents with open physis, showing a striking improvement in knee function without growth arrest and angular deformity of the affected limb in the short-term follow-up.


Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to limitations of ethical approval involving the patient data and anonymity but are available from the corresponding author on a reasonable request.
Abbreviations
- PCL :
-
Posterior cruciate ligament
- ACL :
-
Anterior cruciate ligament
- ACLR :
-
Arthroscopic anterior cruciate ligament reconstruction
- PCLR :
-
Posterior cruciate ligament reconstruction
- ROM :
-
Range of motion
- VAS :
-
Visual analogue scale
- IKDC :
-
International Knee Documentation Committee
- MRI :
-
Magnetic resonance imaging
References
Yoon KH, Lee JH, Kim SG, Park JY, Lee HS, Kim SJ et al (2023) Effect of posterior tibial slopes on graft survival rates at 10 years after primary single-bundle posterior cruciate ligament reconstruction. Am J Sports Med 515:1194–1201
Maniar N, Verhagen E, Bryant AL, Opar DA (2022) Trends in Australian knee injury rates: an epidemiological analysis of 228,344 knee injuries over 20 years. Lancet Reg Health West Pac 21:100409
Seil R, Weitz FK, Pape D (2015) Surgical-experimental principles of anterior cruciate ligament (ACL) reconstruction with open growth plates. J Exp Orthop 21:11
Caine D, DiFiori J, Maffulli N (2006) Physeal injuries in children’s and youth sports: reasons for concern? Br J Sports Med 409:749–760
Kocher MS, Saxon HS, Hovis WD, Hawkins RJ (2002) Management and complications of anterior cruciate ligament injuries in skeletally immature patients: survey of the Herodicus Society and The ACL Study Group. J Pediatr Orthop 224:452–457
Janarv PM, Wikstrom B, Hirsch G (1998) The influence of transphyseal drilling and tendon grafting on bone growth: an experimental study in the rabbit. J Pediatr Orthop 182:149–154
Pierce TP, Issa K, Festa A, Scillia AJ, McInerney VK (2017) Pediatric anterior cruciate ligament reconstruction: a systematic review of transphyseal versus physeal-sparing techniques. Am J Sports Med 452:488–494
Gausden EB, Calcei JG, Fabricant PD, Green DW (2015) Surgical options for anterior cruciate ligament reconstruction in the young child. Curr Opin Pediatr 271:82–91
HamrinSenorski E, Seil R, Svantesson E, Feller JA, Webster KE, Engebretsen L et al (2018) “I never made it to the pros...” Return to sport and becoming an elite athlete after pediatric and adolescent anterior cruciate ligament injury-current evidence and future directions. Knee Surg Sports Traumatol Arthrosc 264:1011–1018
Vavken P, Murray MM (2011) Treating anterior cruciate ligament tears in skeletally immature patients. Arthroscopy 275:704–716
Khakha RS, Yasen SK, Wilson AJ (2018) Paediatric physeal sparing posterior cruciate ligament (PCL) reconstruction with parental donation allograft: rationale and operative approach. Knee 251:203–209
Accadbled F, Knorr J, Sales de Gauzy J (2013) All inside transtibial arthroscopic posterior cruciate ligament reconstruction in skeletally immature: surgical technique and a case report. Orthop Traumatol Surg Res 993:361–365
Bovid KM, Salata MJ, Vander Have KL, Sekiya JK (2010) Arthroscopic posterior cruciate ligament reconstruction in a skeletally immature patient: a new technique with case report. Arthroscopy 264:563–570
Dedouit F, Auriol J, Rousseau H, Rouge D, Crubezy E, Telmon N (2012) Age assessment by magnetic resonance imaging of the knee: a preliminary study. Forensic Sci Int 2171–3(232):e231-237
Rossi MJ, Lubowitz JH, Guttmann D (2002) Development and validation of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med 301:152
Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ (2004) Reliability, validity, and responsiveness of the Lysholm knee scale for various chondral disorders of the knee. J Bone Joint Surg Am 866:1139–1145
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Jung YB, Jung HJ, Song KS, Kim JY, Lee HJ, Lee JS (2010) Remnant posterior cruciate ligament-augmenting stent procedure for injuries in the acute or subacute stage. Arthroscopy 262:223–229
Lee YS, Jung YB (2013) Posterior cruciate ligament: focus on conflicting issues. Clin Orthop Surg 54:256–262
Craddock W, Smithers T, Harris C, du Moulin W, Molnar R (2018) Magnetic resonance imaging of the posterior cruciate ligament in flexion. Knee 253:507–512
Brisson NM, Agres AN, Jung TM, Duda GN (2021) Gait adaptations at 8 years after reconstruction of unilateral isolated and combined posterior cruciate ligament injuries. Am J Sports Med 499:2416–2425
Kumar A, Sinha S, Arora R, Gaba S, Khan R, Kumar M (2021) The 50 top-cited articles on the posterior cruciate ligament: a bibliometric analysis and review. Orthop J Sports Med 911:23259671211057852
Kumar S, Ahearne D, Hunt DM (2013) Transphyseal anterior cruciate ligament reconstruction in the skeletally immature: follow-up to a minimum of sixteen years of age. J Bone Joint Surg Am 951:e1
Kocher MS, Garg S, Micheli LJ (2005) Physeal sparing reconstruction of the anterior cruciate ligament in skeletally immature prepubescent children and adolescents. J Bone Joint Surg Am 8711:2371–2379
Kocher MS, Heyworth BE, Fabricant PD, Tepolt FA, Micheli LJ (2018) Outcomes of physeal-sparing ACL reconstruction with iliotibial band autograft in skeletally immature prepubescent children. J Bone Joint Surg Am 10013:1087–1094
Roberti di Sarsina T, Macchiarola L, Signorelli C, Grassi A, Raggi F, MarcheggianiMuccioli GM et al (2019) Anterior cruciate ligament reconstruction with an all-epiphyseal “over-the-top” technique is safe and shows low rate of failure in skeletally immature athletes. Knee Surg Sports Traumatol Arthrosc 272:498–506
Ahn JH, Yang HS, Jeong WK, Koh KH (2006) Arthroscopic transtibial posterior cruciate ligament reconstruction with preservation of posterior cruciate ligament fibers: clinical results of minimum 2-year follow-up. Am J Sports Med 342:194–204
Dasari SP, Warrier AA, Condon JJ, Mameri ES, Khan ZA, Kerzner B et al (2023) A Comprehensive Meta-analysis of Clinical and Biomechanical Outcomes Comparing Double-Bundle and Single-Bundle Posterior Cruciate Ligament Reconstruction Techniques. Am J Sports Med 5113:3567–3582
Sorensen OG, Fauno P, Christiansen SE, Lind M (2017) Posterior cruciate ligament reconstruction in skeletal immature children. Knee Surg Sports Traumatol Arthrosc 2512:3901–3905
Kocher MS, Smith JT, Zoric BJ, Lee B, Micheli LJ (2007) Transphyseal anterior cruciate ligament reconstruction in skeletally immature pubescent adolescents. J Bone Joint Surg Am 8912:2632–2639
Teng Y, Zhang X, Ma C, Wu H, Li R, Wang H et al (2019) Evaluation of the permissible maximum angle of the tibial tunnel in transtibial anatomic posterior cruciate ligament reconstruction by computed tomography. Arch Orthop Trauma Surg 1394:547–552
Zhang X, Teng Y, Yang X, Li R, Ma C, Wang H et al (2018) Evaluation of the theoretical optimal angle of the tibial tunnel in transtibial anatomic posterior cruciate ligament reconstruction by computed tomography. BMC Musculoskelet Disord 191:436
Gill TJT, Van de Velde SK, Carroll KM, Robertson WJ, Heyworth BE (2012) Surgical technique: aperture fixation in PCL reconstruction: applying biomechanics to surgery. Clin Orthop Relat Res 4703:853–860
Acknowledgements
We would like to thank all the staff in our Department of Orthopedics.
Funding
This work was financially supported by Sichuan Science and Technology Program (Grant No. 2023YFO0009) to Zhong Li.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. ZL and JL designed the study. XL drafted the article. ZL and JL performed the surgery. ZJ and HY revised the manuscript. LL and ZW collected the data. The authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval
The Ethics Committee of the Affiliated Hospital of Southwest Medical University approved all experimental procedures in conformity with the Declaration of Helsinki.
Consent to participate
Written informed consent was obtained from the parents.
Consent for publication
Informed consent for the article publication was obtained from all the patients and their parents in this study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, X., Yang, H., Jun, Z. et al. Outcomes of physeal-sparing posterior cruciate ligament reconstruction for adolescents with an open physis. International Orthopaedics (SICOT) (2023). https://doi.org/10.1007/s00264-023-06037-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00264-023-06037-9