Abstract
Study design
Systematic review.
Introduction
Total hip arthroplasty (THA) is a well-acknowledged surgical intervention to restore a painless and mobile joint in patients with osteoarticular tubercular arthritis of the hip joint. However, there is still substantial uncertainty about the ideal management, clinical and functional outcomes following THA undertaken in patients with acute Mycobacterium tuberculosis (TB) hip infections.
Aim of the study
To undertake a systematic review and evaluate existing literature on patients undergoing THA for acute mycobacterium tuberculosis arthritis of the hip.
Methods
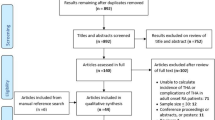
A systematic review of electronic databases of PubMed, EMBASE, Scopus, Web of Science and Cochrane Library was performed on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The search focused on “arthroplasty in cases with tuberculosis of hip joint” since inception of databases until July 2023. Data on patient demographics, clinical characteristics, treatment administered, surgical interventions and outcome, as reported in the included studies, were recorded. Median (range) and mean (standard deviation) were used to summarise the data for continuous variables (as reported in the original studies); and frequency/percentage was employed for categorical variables. Available data on Harris hip scores and complications were statistically pooled using random-effects meta-analysis or fixed-effect meta-analysis, as appropriate
Results
Among a total of 1695 articles, 15 papers were selected for qualitative summarisation and 12 reporting relevant data were included for proportional meta-analysis. A total of 303 patients (mean age: 34 to 52 years; mean follow-up: 2.5 to 10.5 years) were included in our systematic review. In a majority of included studies, postero-lateral approach and non-cemented prosthesis were employed. Fourteen studies described a single-staged procedure in the absence of sinus, abscess and tubercular infection syndrome (TIS). All surgeries were performed under cover of prolonged course of multi-drug anti-tubercular regimen. The mean Harris hip score (HHS) at final follow-up was 91.36 [95% confidence interval (CI): 89.56–93.16; I2:90.44%; p<0.001]. There were 30 complications amongst 174 (9.9%) patients (95% CI: 0.06–0.13; p=0.14; I2=0%).
Conclusion
THA is a safe and effective surgical intervention in patients with active and advanced TB arthritis of hip. It is recommended that the surgery be performed under cover of multi-drug anti-tubercular regimen. In patients with active sinus tracts, abscesses and TIS, surgery may be accomplished in a multi-staged manner. The clinical (range of motion, deformity correction, walking ability and pain scores), radiological (evidence of radiological reactivation and implant incorporation) and function outcome (as assessed by HHS) significantly improve after THA in these patients.



Similar content being viewed by others
References
Moon MS, Kim SS, Lee SR et al (2012) Tuberculosis of hip in children: a retrospective analysis. Indian J Orthop 46(2):191–199. https://doi.org/10.4103/0019-5413.93686
Shanmugasundaram TK (1983) A clinicoradiological classification of tuberculosis of the hip. In: Shanmugasundaram TK (ed) Current concepts in bone and joint tuberculosis. Proceedings of Combined Congress of International Bone and Joint Tuberculosis Club and the Indian Orthop Assoc, Madras, India, p 60
Gautam D, Jain VK, Iyengar KP et al (2021) Total hip arthroplasty in tubercular arthritis of the hip - surgical challenges and choice of implants. J Clin Orthop Trauma 17:214–217. https://doi.org/10.1016/j.jcot.2021.03.018
Viswanathan VK, Subramanian S (2023) Pott Disease. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538331/
Zhang Y, Zhang H (2013) One-stage total joint arthroplasty for patients with active tuberculosis. Orthopedics 36:328–330. https://doi.org/10.3928/01477447-20130426-02
Tiwari A, Karkhur Y, Maini L (2018) Total hip replacement in tuberculosis of hip: a systematic review. J Clin Orthop Trauma 9:54–57. https://doi.org/10.1016/j.jcot.2017.09.013
Neogi DS, Yadav CS, Kumar Ashok, null, et al (2010) Total hip arthroplasty in patients with active tuberculosis of the hip with advanced arthritis. Clin Orthop Relat Res 468:605–612. https://doi.org/10.1007/s11999-009-0957-9
Babhulkar S, Pande S (2002) Tuberculosis of the hip. Clin Orthop Relat Res 93–99. https://doi.org/10.1097/00003086-200205000-00013
Clegg J (1977) The results of the pseudarthrosis after removal of an infected total hip prosthesis. J Bone Joint Surg Br 59:298–301. https://doi.org/10.1302/0301-620X.59B3.893508
Dallari D, Fini M, Carubbi C et al (2011) Total hip arthroplasty after excision arthroplasty: indications and limits. Hip Int 21:436–440. https://doi.org/10.5301/hip.2011.8515
Tuli SM, Mukherjee SK (1981) Excision arthroplasty for tuberculous and pyogenic arthritis of the hip. J Bone Joint Surg Br 63-B:29–32. https://doi.org/10.1302/0301-620X.63B1.7204469
Oztürkmen Y, Karamehmetoğlu M, Leblebici C et al (2010) Cementless total hip arthroplasty for the management of tuberculosis coxitis. Arch Orthop Trauma Surg 130:197–203. https://doi.org/10.1007/s00402-009-0967-9
Sm T, Sk M (1981) Excision arthroplasty for tuberculous and pyogenic arthritis of the hip. The Journal of bone and joint surgery British volume 63-B: https://doi.org/10.1302/0301-620X.63B1.7204469
Wang Q, Shen H, Jiang Y et al (2011) Cementless total hip arthroplasty for the treatment of advanced tuberculosis of the hip. Orthopedics 34:90. https://doi.org/10.3928/01477447-20101221-07
Zeng M, Hu Y, Leng Y et al (2015) Cementless total hip arthroplasty in advanced tuberculosis of the hip. Int Orthop 39:2103–2107. https://doi.org/10.1007/s00264-015-2997-y
Sultan AA, Dalton SE, Umpierrez E et al (2019) Total hip arthroplasty in the setting of tuberculosis infection of the hip: a systematic analysis of the current evidence. Expert Rev Med Devices 16:363–371. https://doi.org/10.1080/17434440.2019.1606710
Kim YH, Han DY, Park BM (1987) Total hip arthroplasty for tuberculous coxarthrosis. J Bone Joint Surg Am 69:718–727
Kim S-J, Postigo R, Koo S, Kim JH (2013) Total hip replacement for patients with active tuberculosis of the hip: a systematic review and pooled analysis. Bone Joint J 95-B:578–582. https://doi.org/10.1302/0301-620X.95B5.31047
Chen C, Yin Y, Xu H, Chen G (2021) Early clinical outcomes of one-stage total hip arthroplasty for the treatment of advanced hip tuberculosis. J Orthop Surg (Hong Kong) 29:23094990211000144. https://doi.org/10.1177/23094990211000143
Hoan DD, Thanh DX, Trang NK, Toan NV (2022) Hip Tuberculosis at stage IV: outcomes and some conditions for total hip replacement. Open Journal of Orthopedics 12:183–194. https://doi.org/10.4236/ojo.2022.124017
Eskola A, Santavirta S, Konttinen YT et al (1988) Cementless total replacement for old tuberculosis of the hip. J Bone Joint Surg Br 70:603–606. https://doi.org/10.1302/0301-620X.70B4.3403606
Yoon TR, Rowe SM, Santosa SB et al (2005) Immediate cementless total hip arthroplasty for the treatment of active tuberculosis. J Arthroplasty 20:923–926. https://doi.org/10.1016/j.arth.2004.08.002
Tan SM, Chin PL (2015) Total hip arthroplasty for surgical management of advanced tuberculous hip arthritis: case report. World J Orthop 6:316–321. https://doi.org/10.5312/wjo.v6.i2.316
Wang Y, Wang J, Xu Z et al (2010) Total hip arthroplasty for active tuberculosis of the hip. Int Orthop 34:1111–1114. https://doi.org/10.1007/s00264-009-0854-6
Singh AP, Singh AP, Mahajan S (2010) Response to “Total hip arthroplasty for active tuberculosis of the hip.” Int Orthop 34:461; author reply 463-464. https://doi.org/10.1007/s00264-009-0876-0
Bhosale PB, Jaiswal R, Purohit S, Arte SM (2021) Total hip arthroplasty in 52 active advanced tubercular arthritic hips. J Arthroplasty 36:1035–1042. https://doi.org/10.1016/j.arth.2020.09.016
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535. https://doi.org/10.1136/bmj.b2535
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n711. https://doi.org/10.1136/bmj.n71
Li L, Chou K, Deng J et al (2016) Two-stage total hip arthroplasty for patients with advanced active tuberculosis of the hip. J Orthop Surg Res 11:38. https://doi.org/10.1186/s13018-016-0364-3
Sidhu AS, Singh AP, Singh AP (2009) Total hip replacement in active advanced tuberculous arthritis. J Bone Joint Surg Br 91:1301–1304. https://doi.org/10.1302/0301-620X.91B10.22541
Raja BS, Ansari S, Yadav R et al (2023) Total hip replacement in active and inactive tuberculosis hip: a systematic review. Indian J Orthop 57:351–370. https://doi.org/10.1007/s43465-023-00817-6
Author information
Authors and Affiliations
Contributions
Vibhu Krishnan Viswanathan: methodology, formal analysis and investigation, writing—original draft preparation. Mohit Kumar Patralekh: conceptualization, methodology, formal analysis and investigation, resources. Guna Pratheep Kalanjiyam: methodology, formal analysis, and investigation. Karthikeyan P Iyengar: conceptualization, methodology, writing—review and editing. Vijay Kumar Jain: conceptualization, methodology, writing—review and editing, resources, supervision.
Corresponding author
Ethics declarations
Consent to participate and publish
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Viswanathan, V.K., Patralekh, M.K., Kalanjiyam, G.P. et al. Total hip arthroplasty in active and advanced tubercular arthritis: a systematic review of the current evidence. International Orthopaedics (SICOT) 48, 79–93 (2024). https://doi.org/10.1007/s00264-023-05943-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05943-2