Abstract
Purpose
The purpose of the study is to determine the efficacy and safety of postoperative single-dose anticoagulant treatment in preventing venous thromboembolism (VTE) after revision THA, in comparison with a multiple-dose chemoprophylaxis protocol.
Methods
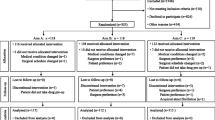
We retrospectively compared 295 patients undergoing revision THA who received multiple-dose chemoprophylaxis protocol (40 mg low-molecular-weight heparin once and oral rivaroxaban for 10 days) or single-dose chemoprophylaxis protocol (40 mg low-molecular-weight heparin once) for VTE. The patients in both groups performed active lower limb exercises. Each group was further stratified into subgroups based on the aetiology of revision. The incidence of VTE, wound complications within three months, hidden blood loss (HBL), transfusion rate, and surgical drainage duration were recorded.
Results
The incidence rates of VTE (P = 0.870) did not differ between the two prophylaxis protocols. However, significant differences were observed in wound complications within three months (P = 0.002), HBL (P = 0.015), transfusion rate (P = 0.028). Surgical drainage duration was also shorter in the single-dose chemoprophylaxis group (P = 0.0023). In the subgroup analysis, the use of single-dose chemoprophylaxis protocol cannot significantly reduce HBL and transfusion rate after septic revision THA. The use of multiple-dose chemoprophylaxis protocol (OR = 2.89, P = 0.002) and high BMI (OR = 1.09, P = 0.037) were independent risk factors of wound complications.
Conclusions
Single-dose chemoprophylaxis protocol effectively and safely prevented VTE after revision THA compared with multiple-dose chemoprophylaxis protocol. The effect in reducing HBL and postoperative transfusion rate was limited in septic revision.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon 304 reasonable request.
References
Sloan M, Premkumar A, Sheth NP (2018) Projected volume of primary total joint arthroplasty in the US, 2014 to 2030. J Bone Joint Surg Am 100(17):1455–1460. https://doi.org/10.2106/JBJS.17.01617
Patel A, Pavlou G, Mújica-Mota RE, Toms AD (2015) The epidemiology of revision total knee and hip arthroplasty in England and Wales: a comparative analysis with projections for the United States. A study using the National Joint Registry dataset. Bone Joint J 97-b(8):1076–1081. https://doi.org/10.1302/0301-620X.97B8.35170
Brenkel IJ, Cook RE (2003) Thromboprophylaxis in patients undergoing total hip replacement. Hosp Med 64(5):281–287. https://doi.org/10.12968/hosp.2003.64.5.1760
Courtney PM, Boniello AJ, Levine BR, Sheth NP, Paprosky WG (2017) Are revision hip arthroplasty patients at higher risk for venous thromboembolic events than primary hip arthroplasty patients? J Arthroplasty 32(12):3752–3756. https://doi.org/10.1016/j.arth.2017.07.028
Chua MJ, Hart AJ, Mittal R, Harris IA, Xuan W, Naylor JM (2017) Early mobilisation after total hip or knee arthroplasty: a multicentre prospective observational study. PLoS One 12(6):e0179820. https://doi.org/10.1371/journal.pone.0179820
Runner RP, Gottschalk MB, Staley CA, Pour AE, Roberson JR (2019) Utilization patterns, efficacy, and complications of venous thromboembolism prophylaxis strategies in primary hip and knee arthroplasty as reported by American Board of Orthopedic Surgery Part II Candidates. J Arthroplasty 34(4):729–734. https://doi.org/10.1016/j.arth.2018.12.015
Badarudeen S, Shu AC, Ong KL, Baykal D, Lau E, Malkani AL (2017) Complications after revision total hip arthroplasty in the Medicare population. J Arthroplasty 32(6):1954–1958. https://doi.org/10.1016/j.arth.2017.01.037
Watts CD, Houdek MT, Wagner ER, Lewallen DG, Mabry TM (2016) Morbidly obese vs nonobese aseptic revision total hip arthroplasty: surprisingly similar outcomes. J Arthroplasty 31(4):842–845. https://doi.org/10.1016/j.arth.2015.08.036
Manista GC, Batko BD, Sexton AC et al (2019) Anticoagulation in revision total joint arthroplasty: a retrospective review of 1917 cases. Orthopedics 42(6):323–329. https://doi.org/10.3928/01477447-20190906-02
Bautista M, Muskus M, Tafur D, Bonilla G, Llinas A, Monsalvo D (2019) Thromboprophylaxis for hip revision arthroplasty: can we use the recommendations for primary hip surgery? A cohort study. Clin Appl Thromb Hemost 25:1076029618820167. https://doi.org/10.1177/1076029618820167
Ji B, Li G, Zhang X, Wang Y, Mu W, Cao L (2021) Multicup reconstruction technique for the management of severe protrusio acetabular defects. Arthroplasty 3(1):26–26. https://doi.org/10.1186/s42836-021-00081-9
Ji B, Zhang X, Xu B, Guo W, Mu W, Cao L (2017) Single-stage revision for chronic fungal periprosthetic joint infection: an average of 5 years of follow-up. J Arthroplasty 32(8):2523–2530. https://doi.org/10.1016/j.arth.2017.03.030
Mu W, Xu B, Guo W, Ji B, Wahafu T, Cao L (2021) Outcome of irrigation and debridement with topical antibiotics delivery for the management of periprosthetic joint infection occurring within 3 months since the primary total joint arthroplasty. J Arthroplasty 36(5):1765–1771. https://doi.org/10.1016/j.arth.2020.11.033
Schulman S, Angerås U, Bergqvist D, Eriksson B, Lassen MR, Fisher W (2010) Definition of major bleeding in clinical investigations of antihemostatic medicinal products in surgical patients. J Thromb Haemost 8(1):202–204. https://doi.org/10.1111/j.1538-7836.2009.03678.x
Nadler SB, Hidalgo JH, Bloch T (1962) Prediction of blood volume in normal human adults. Surgery 51(2):224–232
Sehat KR, Evans R, Newman JH (2000) How much blood is really lost in total knee arthroplasty? - Correct blood loss management should take hidden loss into account. Knee 7(3):151–155. https://doi.org/10.1016/s0968-0160(00)00047-8
Burnett RS, Clohisy JC, Wright RW et al (2007) Failure of the American College of Chest Physicians-1A protocol for lovenox in clinical outcomes for thromboembolic prophylaxis. J Arthroplasty 22(3):317–324. https://doi.org/10.1016/j.arth.2007.01.007
Mills RM, Berkowitz RD, Damaraju CV, Jennings LK, Wildgoose P (2012) Initiation of rivaroxaban following low molecular weight heparin for thromboprophylaxis after total joint replacement: the Safe, Simple Transitions (SST) study. Thromb Res 130(5):709–715. https://doi.org/10.1016/j.thromres.2012.07.014
Wurnig C, Clemens A, Rauscher H et al (2015) Safety and efficacy of switching from low molecular weight heparin to dabigatran in patients undergoing elective total hip or knee replacement surgery. Thromb J 13:37. https://doi.org/10.1186/s12959-015-0066-9
Scuderi GR (2018) Avoiding postoperative wound complications in total joint arthroplasty. J Arthroplasty 33(10):3109–3112. https://doi.org/10.1016/j.arth.2018.01.025
Yamaguchi T, Hasegawa M, Niimi R, Sudo A (2010) Incidence and time course of asymptomatic deep vein thrombosis with fondaparinux in patients undergoing total joint arthroplasty. Thromb Res 126(4):e323-326. https://doi.org/10.1016/j.thromres.2010.03.018
Hanna-Sawires RG, Groen JV, Klok FA et al (2019) Outcomes following pancreatic surgery using three different thromboprophylaxis regimens. Br J Surg 106(6):765–773. https://doi.org/10.1002/bjs.11103
Klingel R, Schwarting A, Lotz J, Eckert M, Hohmann V, Hafner G (2004) Safety and efficacy of single bolus anticoagulation with enoxaparin for chronic hemodialysis. Results of an open-label post-certification study. Kidney Blood Press Res 27(4):211–217. https://doi.org/10.1159/000079866
Runner RP, Shau DN, Staley CA, Roberson JR (2021) Utilization patterns, efficacy, and complications of venous thromboembolism prophylaxis strategies in revision hip and knee arthroplasty as reported by American Board of Orthopaedic Surgery part II candidates. J Arthroplasty 36(7):2364–2370. https://doi.org/10.1016/j.arth.2021.01.072
Jameson SS, Rymaszewska M, James P et al (2012) Wound complications following rivaroxaban administration a multicenter comparison with low-molecular-weight heparins for thromboprophylaxis in lower limb arthroplasty. J Bone Joint Surg Am 94A(17):1554–1558. https://doi.org/10.2106/JBJS.K.00521
Sales CM, Haq F, Bustami R, Sun F (2010) Management of isolated soleal and gastrocnemius vein thrombosis. J Vasc Surg 52(5):1251–1254. https://doi.org/10.1016/j.jvs.2010.05.102
Lotke PA, Steinberg ME, Ecker ML (1994) Significance of deep venous thrombosis in the lower extremity after total joint arthroplasty. Clin Orthop Relat Res 299:25–30
Petersen PB, Lindberg-Larsen M, Jorgensen CC, Kehlet H, Lundbeck Foundation Centre for Fast-track H, Knee Arthroplasty collaborating g (2021) Venous thromboembolism after fast-track elective revision hip and knee arthroplasty - a multicentre cohort study of 2814 unselected consecutive procedures. Thromb Res 199:101–105. https://doi.org/10.1016/j.thromres.2021.01.003
McNally MA, Cooke EA, Mollan RAB (1997) The effect of active movement of the foot on venous blood flow after total hip replacement. J Bone Joint Surg Am 79A(8):1198–1201. https://doi.org/10.2106/00004623-199708000-00012
Bridgens JP, Evans CR, Dobson PMS, Hamer AJ (2007) Intraoperative red blood-cell salvage in revision hip surgery - a case-matched study. J Bone Joint Surg Am 89A(2):270–275. https://doi.org/10.2106/JBJS.F.00492
Aziz S, Almeida K, Taylor G (2021) How should we manage hip fracture patients on direct oral anticoagulants? BMJ Evid Based Med 26(1):22–23. https://doi.org/10.1136/bmjebm-2019-111317
Liu X, Zhang X, Chen Y, Wang Q, Jiang Y, Zeng B (2011) Hidden blood loss after total hip arthroplasty. J Arthroplasty 26(7):1100–1105. https://doi.org/10.1016/j.arth.2010.11.013
Bass AR, Zhang Y, Mehta B et al (2021) Periprosthetic joint infection is associated with an increased risk of venous thromboembolism following revision total knee replacement an analysis of administrative discharge data. J Bone Joint Surg Am 103(14):1312–1318. https://doi.org/10.2106/JBJS.20.01486
Funding
This study was supported by grants from the National Natural Science Foundation of China (No.82260435), and the Natural Science Foundation of Xinjiang (2021D01C331).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Chenghan Chu and Wenbo Mu contributed equally to the work described in the article and share first co-author status. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of First Affiliated Hospital of Xinjiang Medical University (K202208-02).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data and photographs.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The work described in the manuscript is original research that has not been published previously, and the manuscript is not under consideration for publication elsewhere, either in whole or in part.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chu, C., Mu, W., Wahafu, T. et al. Efficacy and safety of postoperative single-dose anticoagulant treatment in preventing venous thromboembolism after revision hip arthroplasty: a retrospective cohort study. International Orthopaedics (SICOT) 47, 2709–2716 (2023). https://doi.org/10.1007/s00264-023-05893-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05893-9