Abstract
Purpose
The anterior cruciate ligament (ACL) is crucial in maintaining knee stability. Some motion mechanisms, which are common in sports, cause excessive load to be passed on the ACL. In non-contact ACL injuries, the ACL cannot sustain the high stress and becomes injured or ruptures in the valgus-external rotation mechanism (VERM) and varus-internal rotation mechanism (VIRM). The mechanical strength of the grafts used to repair the torn ligament varies. The purpose of this study is to look at the alterations in the menisci after anterior cruciate ligament repair with autografts and synthetic grafts in cases of non-contact re-injury mechanisms.
Methods
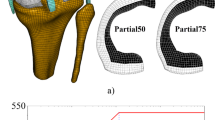
In the finite element analysis, VERM and VIRM motions of the injury were simulated with different ACL graft materials. During the simulations of these mechanism motions with polyethylene terephthalate (PET) and patellar tendon (PT), the contact pressures, contact areas, and von mises stress values created in the medial and lateral meniscus were compared.
Results
The peak contact pressures on the menisci during the VERM are higher than the peak contact pressures during the VIRM, except for one variation. The peak contact pressure of the medial meniscus is almost the same for both graft materials and mechanisms. Furthermore, the peak contact pressures in the menisci are higher than in the VERM. For all injury mechanisms, the peak contact stresses on the lateral meniscus are higher than on the medial meniscus.
Conclusions
The findings suggest that VERM can induce further knee joint injury. It was found that the PET will lessen the pressure on the menisci even more. It is also advantageous since it does not damage the anterior extremities and transmits less pressure to the menisci. In conclusion, using a high-strength ACL is healthier for the menisci. Even though synthetic grafts are not clinically preferred, the study demonstrates that enhancing the material properties of synthetic grafts will increase the chance of their use in the future, based on the current results.







Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
Sanders TL, Maradit Kremers H, Bryan AJ et al (2016) Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med 44:1502–1507. https://doi.org/10.1177/0363546516629944
Ristić V, Ninković S, Harhaji V, Milankov M (2010) Causes of anterior cruciate ligament injuries. Med Pregl 63:541–545. https://doi.org/10.2298/MPNS1008541R
Salem HS, Shi WJ, Tucker BS et al (2018) Contact versus noncontact anterior cruciate ligament injuries: is mechanism of injury predictive of concomitant knee pathology? Arthroscopy 34:200–204
Colby S, Francisco A, Yu B et al (2000) Electromyographic and kinematic analysis of cutting maneuvers. Implications for anterior cruciate ligament injury. Am J Sports Med 28:234–240. https://doi.org/10.1177/03635465000280021501
Arilla FV, Yeung M, Bell K et al (2015) Experimental execution of the simulated pivot-shift test: a systematic review of techniques. Arthroscopy 31:2445–2454.e2. https://doi.org/10.1016/j.arthro.2015.06.027
Yagi M, Wong EK, Kanamori A et al (2002) Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med 30:660–666. https://doi.org/10.1177/03635465020300050501
Brouwer GM, van Tol AW, Bergink AP et al (2007) Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis Rheum 56:1204–1211. https://doi.org/10.1002/art.22515
Cerejo R, Dunlop DD, Cahue S et al (2002) The influence of alignment on risk of knee osteoarthritis progression according to baseline stage of disease. Arthritis Rheum 46:2632–2636. https://doi.org/10.1002/art.10530
Sharma L, Eckstein F, Song J et al (2008) Relationship of meniscal damage, meniscal extrusion, malalignment, and joint laxity to subsequent cartilage loss in osteoarthritic knees. Arthritis Rheum 58:1716–1726. https://doi.org/10.1002/art.23462
Canale ST (2003) Campbell’s Operative Orthopaedics. In: Miller RH (ed) Knee Injuries, 10th edn. Mosby-Yearbook, Philadelphia, pp 2165–2338
Gür S (1999) Greft Seçimi. Acta Orthopaedica et Traumatologica Turcica 33:401–404
Insall JN, Scott WN (2001) Surgery of the Knee. Classification of the knee ligament injury, 3rd edn. Churchill Livingstone, Philadelphia, pp 585–595
Nicholas JA (1970) Injuries to knee ligaments. Relationship to looseness and tightness in football players. JAMA 212:2236–2239. https://doi.org/10.1001/jama.212.13.2236
Cihan S, Duman E (2020) Ön Çapraz Bağ Rekonstrüksiyonunda Transtibial ve Anteromedial Portal Tekniklerin Fonksiyonel Olarak Karşılaştırılması. Turkish J Clin Lab 412–418. https://doi.org/10.18663/tjcl.822342
Shelton WR, Fagan BC (2011) Autografts commonly used in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg 19:259–264. https://doi.org/10.5435/00124635-201105000-00003
Cheung SC, Allen CR, Gallo RA et al (2012) Patients’ attitudes and factors in their selection of grafts for anterior cruciate ligament reconstruction. Knee 19:49–54. https://doi.org/10.1016/j.knee.2010.11.009
West RV, Harner CD (2005) Graft selection in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg 13:197–207. https://doi.org/10.5435/00124635-200505000-00006
Dhammi IK, Ul-Haq R, Kumar S (2015) Graft choices for anterior cruciate ligament reconstruction. Indian J Orthop 49:127–128. https://doi.org/10.4103/0019-5413.152393
Macaulay AA, Perfetti DC, Levine WN (2012) Anterior cruciate ligament graft choices. Sports Health 4:63–68. https://doi.org/10.1177/1941738111409890
Shaerf DA, Pastides PS, Sarraf KM, Willis-Owen CA (2014) Anterior cruciate ligament reconstruction best practice: a review of graft choice. World J Orthop 5:23–29. https://doi.org/10.5312/wjo.v5.i1.23
Legnani C, Ventura A, Terzaghi C et al (2010) Anterior cruciate ligament reconstruction with synthetic grafts. A review of literature. Int Orthop 34:465–471. https://doi.org/10.1007/s00264-010-0963-2
Conte EJ, Hyatt AE, Gatt CJJ, Dhawan A (2014) Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure. Arthroscopy 30:882–890. https://doi.org/10.1016/j.arthro.2014.03.028
Tampere T, Devriendt W, Cromheecke M et al (2019) Tunnel placement in ACL reconstruction surgery: smaller inter-tunnel angles and higher peak forces at the femoral tunnel using anteromedial portal femoral drilling—a 3D and finite element analysis. Knee Surg Sports Traumatol Arthrosc 27:2568–2576. https://doi.org/10.1007/s00167-018-5272-0
Otake N, Chen H, Yao X, Shoumura S (2007) Morphologic study of the lateral and medial collateral ligaments of the human knee. Okajimas Folia Anat Jpn 83:115–122. https://doi.org/10.2535/ofaj.83.115
Kubicek M, Florian Z, k, (2009) Stress strain analysis of knee joint. Eng Mech 16:315–322
Park Y-S, Kwon H-B (2013) Three-dimensional finite element analysis of implant-supported crown in fibula bone model. J Adv Prosthodont 5:326–332. https://doi.org/10.4047/jap.2013.5.3.326
Smith RDJ, Zargar N, Brown CP et al (2017) Characterizing the macro and micro mechanical properties of scaffolds for rotator cuff repair. J Shoulder Elbow Surg 26:2038–2046. https://doi.org/10.1016/j.jse.2017.06.035
Wilson TW, Zafuta MP, Zobitz M (1999) A biomechanical analysis of matched bone-patellar tendon-bone and double-looped semitendinosus and gracilis tendon grafts. Am J Sports Med 27:202–207. https://doi.org/10.1177/03635465990270021501
Smeets K, Slane J, Scheys L et al (2017) Mechanical analysis of extra-articular knee ligaments. Part one: native knee ligaments. Knee 24:949–956. https://doi.org/10.1016/j.knee.2017.07.013
Wang H, Zhang M, Cheng C-K (2020) A novel protection liner to improve graft-tunnel interaction following anterior cruciate ligament reconstruction: a finite element analysis. J Orthop Surg Res 15:232. https://doi.org/10.1186/s13018-020-01755-x
Zhu J, Marshall B, Tang X et al (2022) ACL graft with extra-cortical fixation rotates around the femoral tunnel aperture during knee flexion. Knee Surg Sports Traumatol Arthrosc 30:116–123. https://doi.org/10.1007/s00167-021-06703-8
Yin L, Chen K, Guo L et al (2015) Identifying the functional flexion-extension axis of the knee: an in-vivo kinematics study. PLoS One 10:e0128877. https://doi.org/10.1371/journal.pone.0128877
Boguszewski DV, Joshi NB, Yang PR et al (2016) Location of the natural knee axis for internal-external tibial rotation. Knee 23:1083–1088. https://doi.org/10.1016/j.knee.2015.11.003
Wan C, Hao Z, Wen S (2013) The effect of the variation in ACL constitutive model on joint kinematics and biomechanics under different loads: a finite element study. J Biomech Eng 135. https://doi.org/10.1115/1.4023696
Safari M, Shojaei S, Tehrani P, Karimi A (2020) A patient-specific finite element analysis of the anterior cruciate ligament under different flexion angles. J Back Musculoskelet Rehabil 33:811–815. https://doi.org/10.3233/BMR-191505
Huang R, Zheng H, Xu Q (2012) Biomechanical evaluation of different techniques in double bundle anterior cruciate ligament reconstruction using finite element analysis. J Biomim Biomater Tissue Eng 13:55–68. https://doi.org/10.4028/www.scientific.net/JBBTE.13.55
You M-W, Park JS, Park SY et al (2014) Posterior root of lateral meniscus: the detailed anatomic description on 3T MRI. Acta Radiol 55:359–365. https://doi.org/10.1177/0284185113496677
Forkel P, Petersen W (2012) Posterior root tear fixation of the lateral meniscus combined with arthroscopic ACL double-bundle reconstruction: technical note of a transosseous fixation using the tibial PL tunnel. Arch Orthop Trauma Surg 132:387–391. https://doi.org/10.1007/s00402-011-1429-8
De SAA, Blankenbaker DG, Richard K et al (2009) MR diagnosis of posterior root tears of the lateral meniscus using arthroscopy as the reference standard. AJR Am J Roentgenol 192:480–486. https://doi.org/10.2214/AJR.08.1300
Brody JM, Lin HM, Hulstyn MJ, Tung GA (2006) Lateral meniscus root tear and meniscus extrusion with anterior cruciate ligament tear. Radiology 239:805–810. https://doi.org/10.1148/radiol.2393050559
Willinger L, Lang JJ, Berthold D et al (2020) Varus alignment aggravates tibiofemoral contact pressure rise after sequential medial meniscus resection. Knee Surg Sports Traumatol Arthrosc 28:1055–1063. https://doi.org/10.1007/s00167-019-05654-5
Willinger L, Foehr P, Achtnich A et al (2019) Effect of lower limb alignment in medial meniscus-deficient knees on tibiofemoral contact pressure. Orthop J Sports Med. https://doi.org/10.1177/2325967118824611
Donahue TLH, Hull ML, Rashid MM, Jacobs CR (2002) A finite element model of the human knee joint for the study of tibio-femoral contact. J Biomech Eng 124:273–280. https://doi.org/10.1115/1.1470171
Sakamoto Y, Tsukada H, Sasaki S et al (2020) Effects of the tibial tunnel position on knee joint stability and meniscal contact pressure after double-bundle anterior cruciate ligament reconstruction. J Orthop Sci 25:1040–1046. https://doi.org/10.1016/j.jos.2019.12.006
Asano T, Akagi M, Nakamura T (2005) The functional flexion-extension axis of the knee corresponds to the surgical epicondylar axis: in vivo analysis using a biplanar image-matching technique. J Arthroplasty 20:1060–1067. https://doi.org/10.1016/j.arth.2004.08.005
Liu C, Wang Y, Li Z et al (2018) Tibiofemoral joint contact area and stress after single-bundle anterior cruciate ligament reconstruction with transtibial versus anteromedial portal drilling techniques. J Orthop Surg Res 13:247. https://doi.org/10.1186/s13018-018-0956-1
Mulcahey MK, Monchik KO, Yongpravat C et al (2012) Effects of single-bundle and double-bundle ACL reconstruction on tibiofemoral compressive stresses and joint kinematics during simulated squatting. Knee 19:469–476
Cheng R, Wang H, Dimitriou D et al (2022) Central femoral tunnel placement can reduce stress and strain around bone tunnels and graft more than anteromedial femoral tunnel in anterior cruciate ligament reconstruction. Int J Numer Method Biomed Eng 38:e3590. https://doi.org/10.1002/cnm.3590
Acknowledgements
The authors would like to thank Ayberk Dizdar for their contributions to sharing technical information.
Author information
Authors and Affiliations
Contributions
These authors contributed equally to this work.
Corresponding author
Ethics declarations
Ethical approval
Patient’s informed consent and Institutional Review Board approval were obtained before initiating this study (2009/2 KÜ İAEK 1/9).
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Çakır, G.H., Mutlu, İ. A comparison of stress, contact pressure, and contact area on menisci in re-injury mechanisms after reconstruction of the anterior cruciate ligament with autograft and synthetic graft: a finite element study. International Orthopaedics (SICOT) 47, 2487–2496 (2023). https://doi.org/10.1007/s00264-023-05881-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05881-z