Abstract
Purpose
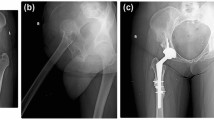
Developmental dysplasia of the hip is still a prevailing secondary cause of early hip osteoarthritis in Jordan. Dysplastic coxarthrosis can result in significant and disabling hip pain with impaired patient’s functionality. Due to this significant morbidity, patients ultimately need total hip arthroplasty, which offers the best functional outcome. Significant anatomical aberrances do exist in such hips as a result of old dysplasia; such pathoanatomical changes can complicate an already difficult surgery and lead to significant intraoperative blood loss and haemoglobin drop postoperatively. So, the aim of this research was to investigate on the intraoperative blood loos, and postoperative haemoglobin drop in these patients.
Methods
A cross-sectional study design was adopted, and 162 patients with advanced hip osteoarthrosis secondary to developmental dysplasia of the hip (DDH) were studied. We studied predictors of hemoglobin drop and blood loss and linked some variables to this outcome variable using different statistical tests.
Results
Our results showed a positive correlation between blood loss and BMI (r = 0.27, p = 0.73), haemoglobin drop and duration of surgery (r = 0.14, p = 0.07), length of hospital stay and duration of surgery (r = 0.25, p = 0.001). No significant differences between outcome measures (blood loss, haemoglobin drop, and duration of surgery) between males and females (p = 0.38, 0.93, 0.77 respectively). However, there was a statistically significant differences in haemoglobin drop among patients underwent general versus spinal anaesthesia (p = 0.03). additionally, there was a statistically significant association in length of hospital stay among smokers (p = 0.03), and patients who didn’t prescribed anxiolytic preoperatively (p = 0.008).
Conclusion
Haemoglobin drop and blood loss in patients with dysplastic coxarthrosis were linked to increased preoperative BMI. Use of preoperative anxiolytics, and being non-smoker decreased the length of hospital stays. General anaesthesia was associated with more haemoglobin drop as well.



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available but may be made available from the corresponding author on reasonable request.
Code availability
Not applicable.
Abbreviations
- DDH:
-
Developmental Dysplasia of the Hip
- THA:
-
Total Hip Arthroplasty
References
Nandhagopal T, De Cicco FL (2022) Developmental Dysplasia Of The Hip. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK563157/
Moraleda L, Albiñana J, Salcedo M, Gonzaléz-Morán G (2013) Dysplasia in the development of the hip. Rev Esp Cir Ortopédica Traumatol (English Ed) 57(1):67–77. https://doi.org/10.1016/J.RECOTE.2013.01.009
Papachristou GC, Pappa E, Chytas D, Masouros PT, Nikolaou VS (2021) Total hip replacement in developmental hip dysplasia: a narrative review. Cureus 13(4):e14763. https://doi.org/10.7759/CUREUS.14763
Atilla B (2016) Reconstruction of neglected developmental dysplasia by total hip arthroplasty with subtrochanteric shortening osteotomy. EFORT Open Rev 1(3):65. https://doi.org/10.1302/2058-5241.1.000026
Vaquero-Picado A, González-Morán G, Garay EG, Moraleda L (2019) Developmental dysplasia of the hip: update of management. EFORT Open Rev 4(9):548–556. https://doi.org/10.1302/2058-5241.4.180019
Farrow L, Faulkner A, Gardner WT, Reidy M (2020) Surgical management for developmental dysplasia of the hip. Orthop Trauma 34(6):324–331. https://doi.org/10.1016/J.MPORTH.2020.09.001
Faldini C et al (2011) Congenital hip dysplasia treated by total hip arthroplasty using cementless tapered stem in patients younger than 50 years old: results after 12-years follow-up. J Orthop Traumatol 12(4):213. https://doi.org/10.1007/S10195-011-0170-Y
Foye PM, Stitik TP (2008) Hip osteoarthritis. In: Essentials of physical medicine and rehabilitation, pp 271–276. https://doi.org/10.1016/B978-1-4160-4007-1.50050-X
Greber EM, Pelt CE, Gililland JM, Anderson MB, Erickson JA, Peters CL (2017) Challenges in total hip arthroplasty in the setting of developmental dysplasia of the hip. J Arthroplasty 32(9S):S38–S44. https://doi.org/10.1016/J.ARTH.2017.02.024
Bozek M, Bielecki T, Nowak R, Zelawski M (2013) Arthroplasty in patients with congenital hip dysplasia – early evaluation of a treatment method. Ortop Traumatol Rehabil 15(1):49–59. https://doi.org/10.5604/15093492.1032794
Yuan L, Bao NR, Zhao JN (2015) Progress on hidden blood loss after hip replacement. Zhongguo Gu Shang 28(4):378–382
Jawad MU, Scully SP (2011) In Brief: Crowe’s Classification: arthroplasty in developmental dysplasia of the hip. Clin Orthop Relat Res 469(1):306. https://doi.org/10.1007/S11999-010-1316-6
Knight SR, Aujla R, Biswas SP (2011) Total Hip Arthroplasty - over 100 years of operative history. Orthop Rev (Pavia) 3(2):16. https://doi.org/10.4081/OR.2011.E16
Varacallo M, Luo TD, Johanson NA (2022) Total Hip Arthroplasty Techniques. StatPearls. Available: https://www.ncbi.nlm.nih.gov/books/NBK507864/. Accessed 3 Jan 2023
Learmonth ID, Young C, Rorabeck C (2007) The operation of the century: total hip replacement. Lancet (London, England) 370(9597):1508–1519. https://doi.org/10.1016/S0140-6736(07)60457-7
Tilbury C et al (2016) Outcome of total hip arthroplasty, but not of total knee arthroplasty, is related to the preoperative radiographic severity of osteoarthritis. A prospective cohort study of 573 patients. Acta Orthop 87(1):67–71. https://doi.org/10.3109/17453674.2015.1092369
Bailey A et al (2021) Preoperative anemia in primary arthroplasty patients-prevalence, influence on outcome, and the effect of treatment. J Arthroplasty 36(7):2281–2289. https://doi.org/10.1016/J.ARTH.2021.01.018
Kunz JV, Spies CD, Bichmann A, Sieg M, Mueller A (2020) Postoperative anaemia might be a risk factor for postoperative delirium and prolonged hospital stay: A secondary analysis of a prospective cohort study. PLoS One 15(2):e0229325. https://doi.org/10.1371/JOURNAL.PONE.0229325
Ye M, Zhou J, Chen J, Yan L, Zhu X (2020) Analysis of hidden blood loss and its influential factors in myomectomy. J Int Med Res 48(5):300060520920417. https://doi.org/10.1177/0300060520920417
Liu X, Zhang X, Chen Y, Wang Q, Jiang Y, Zeng B (2011) Hidden blood loss after total hip arthroplasty. J Arthroplasty 26(7):1100-5.e1. https://doi.org/10.1016/J.ARTH.2010.11.013
Zhao J, Li J, Zheng W, Liu D, Sun X, Xu W (2014) Low body mass index and blood loss in primary total hip arthroplasty: results from 236 consecutive ankylosing spondylitis patients. Biomed Res Int 2014:742393. https://doi.org/10.1155/2014/742393
Bell TH et al (2022) Factors affecting perioperative blood loss and transfusion rates in primary total joint arthroplasty: a prospective analysis of 1642 patients. Can J Surg 52(4):295 [Online]. Available: /pmc/articles/PMC2724803/
Bedard NA, Dowdle SB, Wilkinson BG, Duchman KR, Gao Y, Callaghan JJ (2018) What is the impact of smoking on revision total knee arthroplasty? J Arthroplasty 33(7S):S172–S176. https://doi.org/10.1016/J.ARTH.2018.03.024
Matharu GS et al (2019) The effect of smoking on outcomes following primary total hip and knee arthroplasty: a population-based cohort study of 117,024 patients. Acta Orthop 90(6):559–567. https://doi.org/10.1080/17453674.2019.1649510/SUPPL_FILE/IORT_A_1649510_SM1781.PDF
Yue C et al (2022) Associations between smoking and clinical outcomes after total hip and knee arthroplasty: a systematic review and meta-analysis. Front Surg 9:1766. https://doi.org/10.3389/FSURG.2022.970537/BIBTEX
Meldrum RD, Wurtz LD, Feinberg JR, Capello WN (2005) Does smoking affect implant survivorship in total hip arthroplasty?: a preliminary retrospective case series. Iowa Orthop J 25:17. [Online]. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888760/. Accessed 03 Jan 2023
Teng S, Yi C, Krettek C, Jagodzinski M (2015) Smoking and risk of prosthesis-related complications after total hip arthroplasty: a meta-analysis of cohort studies. PLoS One 10(4):e0125294. https://doi.org/10.1371/JOURNAL.PONE.0125294
“Survival of hip replacements. A comparison of a randomized trial and a registry - PubMed.” https://pubmed.ncbi.nlm.nih.gov/10853165/. Accessed 03 Jan 2023
Rolfson O, Dahlberg LE, Nilsson JÅ, Malchau H, Garellick G (2009) Variables determining outcome in total hip replacement surgery. J Bone Jt Surg Ser B 91(2):157–161. https://doi.org/10.1302/0301-620X.91B2.20765/ASSET/IMAGES/LARGE/20765-2.JPEG
Greene ME, Rolfson O, Gordon M, Annerbrink K, Malchau H, Garellick G (2016) Is the use of antidepressants associated with patient-reported outcomes following total hip replacement surgery? Acta Orthop 87(5):444. https://doi.org/10.1080/17453674.2016.1216181
Rajamäki TJ, Moilanen T, Puolakka PA, Hietaharju A, Jämsen E (2021) Is the preoperative use of antidepressants and benzodiazepines associated with opioid and other analgesic use after hip and knee arthroplasty? Clin Orthop Relat Res 479(10):2268–2280. https://doi.org/10.1097/CORR.0000000000001793
Seagrave KG, Lewin AM, Harris IA, Badge H, Naylor J (2021) Association between pre-operative anxiety and/or depression and outcomes following total hip or knee arthroplasty. J Orthop Surg (Hong Kong) 29(1):2309499021992605. https://doi.org/10.1177/2309499021992605
Acknowledgements
The authors appreciate the technical support of all the radiology staff.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study's conception and design. Material preparation, data collection, and analysis were performed by Saba AlNsours, Sohayla Dababseh, Mohammad A. Alsmairat. The first draft of the manuscript was written by Moh'd S. Dawod and all authors commented on previous versions of the manuscript. The analysis was done by Mohammed Alshrouf. The discussion section, the conclusion, and the abstract were done by Mohammad Alswerki. Bassem Haddad and Jihad Aljlouni revised the new manuscript, and Mohammad Alswerki made the revisions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Mutah University (IRB no. 912022).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
The authors affirm that human research participants provided informed consent for publication of the results of this research.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of Evidence: Level IV, Cross sectional descriptive study
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dawod, M.S., Alswerki, M.N., Haddad, B.I. et al. Intraoperative blood loss and haemoglobin drop in patients with developmental dysplasia of the hip in Jordan undergoing total hip arthroplasty. International Orthopaedics (SICOT) 47, 2933–2940 (2023). https://doi.org/10.1007/s00264-023-05869-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05869-9